Single-Ingredient Antivirals for the Treatment of HIV-1 PDF
Preview Single-Ingredient Antivirals for the Treatment of HIV-1
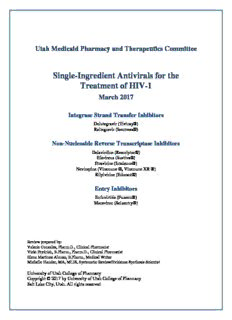
Utah Medicaid Pharmacy and Therapeutics Committee Single-Ingredient Antivirals for the Treatment of HIV-1 March 2017 Integrase Strand Transfer Inhibitors Dolutegravir (Tivicay®) Raltegravir (Isentress®) Non-Nucleoside Reverse Transcriptase Inhibitors Delavirdine (Rescriptor®) Efavirenz (Sustiva®) Etravirine (Intelence®) Nevirapine (Viramune ®, Viramune XR ®) Rilpivirine (Edurant®) Entry Inhibitors Enfuvirtide (Fuzeon®) Maraviroc (Selzentry®) Review prepared by: Valerie Gonzales, Pharm.D., Clinical Pharmacist Vicki Frydrich, B.Pharm., Pharm.D., Clinical Pharmacist Elena Martinez Alonso, B.Pharm., Medical Writer Michelle Fiander, MA, MLIS, Systematic Review/Evidence Synthesis Scientist University of Utah College of Pharmacy Copyright © 2017 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved Table of Contents EXECUTIVE SUMMARY 3 INTRODUCTION 6 Table 1. Single-Ingredient INSTI, NNRTI, and EI Products FDA-Approved for the Treatment of HIV-1 7 DISEASE OVERVIEW 10 PHARMACOLOGY 14 Table 2. Guidelines for HIV-1 Management with Antiretroviral Therapy 11 INTEGRASE STRAND TRANSFER INHIBITORS 14 NON-NUCLEOSIDE REVERSE TRANSCRIPTASE INHIBITORS 14 ENTRY INHIBITORS 15 Table 3. Pharmacokinetics of Single-Ingredient INSTI, NNRTI, and EI Products FDA-Approved for the SPECIAL POPULATIONS 19 Treatment of HIV-1 16 INTEGRASE STRAND TRANSFER INHIBITORS 19 NON-NUCLEOSIDE REVERSE TRANSCRIPTASE INHIBITORS 19 ENTRY INHIBITORS 20 METHODS 25 Table 4. Single-Ingredient INSTI, NNRTI, and EI Products: Applications in Special Populations 21 CLINICAL EFFICACY AND SAFETY— INTEGRASE STRAND TRANSFER INHIBITORS 26 CLINICAL EFFICACY AND SAFETY— NON-NUCLEOSIDE REVERSE TRANSCRIPTASE INHIBITORS 27 CLINICAL EFFICACY AND SAFETY— ENTRY INHIBITORS 30 Table 5. Single-Ingredient INSTI, NNRTI, and EI Products: Common Adverse Effects, SUMMARY 34 Warnings/Precautions, and Safety Comparison 31 APPENDIX A 35 Table 1. FDA-Approved Antiretroviral Agents for the Treatment of HIV-1 35 APPENDIX B 37 Table 2. Timing Concerns for Antiretroviral Therapy Initiation 36 Table 1. MEDLINE & EMBASE Literature Search Strategies for NNRTI Drug Class 37 APPENDIX C 43 Table 2. MEDLINE & EMBASE Literature Search Strategies for INSTI and EI Drug Classes 40 Table 1. Evidence for the Integrase Strand Transfer Inhibitor Drug Class 43 REFERENCES 51 Table 2. Evidence for the Non-Nucleoside Reverse Transcriptase Inhibitor Drug Class 45 2 Executive Summary Introduction Treatment strategies for human immunodeficiency virus (HIV) must be fortified to maintain pace with the virus’s rapid rate of resistance development. The standard of care for initial therapy is a 3-drug : containing regimen, employing agents from at least two different drug classes. Selection of the regimen is guided by pre-treatment resistance testing and carefully tailored to the patient’s comorbidities, co-infections, and concurrent medications. The goals of therapy include preserving and improving the patient’s immunologic function, along with aiming to suppress the plasma HIV load below detectable levels. The rate of newly-diagnosed cases in Utah during 2015 was 4 per 100,000 populations. With regard to children age 13 or younger, nine newly diagnosed cases were reported in Utah between 2005 and 2014. Data from 2013 last cited the prevalence of HIV cases in Utah to be 2,565 persons. This review evaluates the safety and efficacy of the single-active-ingredient containing products based on meta- analyses and randomized controlled trials (RCTs) assessing intra-class comparisons among the integrase strand transfer inhibitors (INSTIs), dolutegravir and elvitegravir; the non-nucleoside reverse transcriptase inhibitors (NNRTIs), delavirdine, efavirenz, etravirine, nevirapine and rilpivirine; and the entry inhibitors (EIs), enfuvirtide and maraviroc, used for the treatment of HIV-1 infection. The single-ingredient elvitegravir product, Vitekta®, was recently removed from the market in February 2017 due to low utilization. Within these drug classes, efavirenz, rilpivirine, dolutegravir, and elvitegravir are also available in complete-regimen combination products. According to the Department of Health and Human Services (DHHS) treatment guideline for HIV-1 infected, treatment-naïve patients, the place in therapy for these three drug classes is as follows: • Integrase Strand Transfer Inhibitors: All INSTIs are recommended as options among preferred initial combination regimens for adults and children. • Non-Nucleoside Reverse Transcriptase Inhibitors: Two of the NNRTIs, efavirenz and rilpivirine, are recommended among alternative-line regimens in adults and adolescents; nevirapine is not recommended in these two populations, however, is a second-line option for certain children. Etravirine is reserved for treatment-experienced patients and delavirdine is no longer recommended among the DHHS guidelines. • Entry Inhibitors: The entry inhibitors are not recommended for initial therapy and are reserved for salvage therapy in treatment-experience patients. A thorough evaluation of virological failure should be carried out for patients experiencing a decline in drug- response. For these patients, an entirely new antiretroviral (ARV) regimen including at least two, preferably three, fully-active agents should be employed as salvage therapy and is guided by the patient’s resistance analysis with expert advice. INSTI Clinical Efficacy & Safety: The efficacy and safety of dolutegravir (DTG) versus raltegravir (RAL) has been compared in two randomized controlled trials (SRING-2 and SAILING), each with different patient populations with respect to ARV-experience. A meta-analysis pooled data from these two trials. In addition, a network meta- analysis indirectly compared these two agents through efavirenz as a common comparator node. In the treatment-naive population, the virological efficacy of DTG was non-inferior to RAL at both 48 and 96 weeks. For the treatment-experienced population, the efficacy of DTG treatment was marginally superior compared to RAL. Although the two meta-analyses only included a small number of trials comparing DTG versus RAL, their findings support the results of the randomized-controlled trials (RCTs), with respect to the experimental population’s ARV-experience. With regard to safety, dolutegravir and raltegravir are comparable with respect to adverse events and discontinuation rates. Commonly reported side effects include diarrhea, upper respiratory tract infection, and 3 headache. In RCTs, rates of discontinuation due to adverse events (AEs) were similar and infrequent in both experimental arms (less than 4%). Reported central nervous system (CNS) adverse events were dizziness, depression, insomnia, and anxiety; the SPRING-2 study found these to be similar between treatment arms, with rates less than 6%. The meta-analyses, reported no difference in serious drug-related AEs or discontinuations due to adverse events at 48 weeks. In the RCTs, comparable, clinically-insignificant lipid effects were observed between the DTG and RAL regimens, suggesting overall that these two agents have a neutral effect on lipids. NNRTI Clinical Efficacy & Safety Comparing the efficacy of efavirenz (EFV) to nevirapine (NVP), three meta- analyses found that nevirapine demonstrates similar virological success in initial ARV treatment. Meta-analyses : found contradictory results with respect to virological failure; one found no difference between EFV and NVP and another found a significant difference in favor of EFV. In addition, two meta-analyses report resistance development to be significantly lower for EFV. One meta-analysis evaluated rash events and found no differences. Two meta-analyses resulted in conflicting outcomes regarding a difference in CNS risk. NVP was found more likely to raise transaminases and cause neutropenia where evaluated in a meta-analysis. Overall, the DHHS guideline recommends EFV in alternative-line options and has reserved recommending NVP-based regimens in adult and adolescents due to its associated risks of fatal hepatotoxicity and hypersensitivity reactions, in addition to having a history of failing to demonstrate non-inferiority with respect to EFV in several RCTs. Nonetheless, both nevirapine and efavirenz have a place in therapy for children according to the DHHS guideline. Comparing the efficacy of efavirenz to rilpivirine (RPV), a meta-analysis found no difference in viral response or change in baseline CD4 count at 48 weeks between EFV and RPV based regimens. A higher virological failure rate in the RPV group was identified. Results from more recent RCTs have demonstrated RPV to be non-inferior to EFV, however, in two subgroups, 1) with a baseline HIV RNA > 100,000 copies/mL and 2) with a baseline CD4 count<200 cells/mL, RPV failed to demonstrate non-inferiority when used as the single-ingredient containing product. Two meta-analyses addressing safety arrived at different conclusions with respect to CNS adverse events comparing EFV to RPV. One showed a lower risk of rash and pooled neurological events with RPV compared to EFV. These differences have also been demonstrated in more recent RCTs than these two meta- analyses, suggesting EFV treatment leads to higher occurrences of both CNS side effects and rash compared to RPV. Overall, randomized-controlled trials were in favor of RPV with respect to changes lipid measures. There were no head-to-head studies meeting inclusion/exclusion criteria that directly compared NVP versus RPV or etravirine and delavirdine versus another NNRTI. Etravirine is indicated for treatment-experienced patients and the DHHS comments that there is insufficient evidence to support its use in treatment-naïve patients. The DHHS guidelines do not recommend delavirdine due to its inferior virological efficacy compared to preferred regimens. The package insert warns of insufficient data comparing delavirdine regimens with currently preferred 3-drug regimens for initial treatment, in addition to mentioning its low performance and durability against 2- drug suboptimal regimens. EI Clinical Efficacy & Safety There were no head-to-head studies found comparing the efficacy of the two FDA- approved entry inhibitors, maraviroc and enfuvirtide. The prescribing-information product insert highlights that : injection-site reactions with enfuvirtide are common, occurring in 98% of patients treated in RCTs leading to the drug’s approval. Furthermore, administration with the needleless Biojector® system may result in neuralgia and/or paresthesia, and hematomas. The most common adverse events reported in the prescribing information for maraviroc are upper respiratory tract infections, cough, pyrexia, rash, dizziness, flatulence, bloating, and gastrointestinal atonic/hypomotility disorders. 4 Summary INSTIs: Of the single-ingredient INSTIs, dolutegravir is dosed once daily and has activity against some HIV strains resistant to raltegravir. Raltegravir is dosed twice daily and is the preferred INSTI during pregnancy. In the treatment-naive population, the virological efficacy of dolutegravir was non-inferior to raltegravir at both 48 and 96 weeks. For the treatment-experienced population, in addition to being non-inferior, DTG treatment resulted in a marginally superior virological-success efficacy compared to the raltegravir arm. With regard to safety, dolutegravir and raltegravir have comparable adverse event and discontinuation rates. All INSTIs are recommended as first-line options among initial ARV combination regimens. They are well-tolerated and have demonstrated durable efficacy and favorable toxicity profiles. NNRTIs: Both efavirenz and rilpivirine are recommended as alternative-line therapies for treatment-naïve adults. Nevirapine is not recommended for adults, however, it is indicated/recommended in some pediatric age groups. Meta-analyses report that NVP and RPV have similar efficacy compared to EFV in terms of virological success in initial HIV treatment. However, NVP has failed to meet non-inferiority in several RCTs; thus, the DHHS guideline reserves recommending it for adults and adolescents. Compared to efavirenz, rilpivirine has shortcomings for the subpopulation with a baseline HIV RNA >100,000 copies/mL or with a baseline CD4 count <200 cells/mL. Recent RCTs suggest RPV results in less rash and CNS toxicity compared to EFV. EFV and NVP rash risks are probably similar, however, NVP has a boxed warning for life-threatening hypersensitivity reactions. Nevirapine is also associated with an increased risk of neutropenia and elevated transaminases compared to efavirenz. No head-to-head intra-class comparison trials were identified for etravirine or delavirdine. Etravirine is indicated for HIV-1-infected treatment-experienced patients with resistance to other NNRTIs, since it has a higher barrier to resistance. There is insufficient evidence to support its use in treatment-naïve patients. The DHHS does not recommend delavirdine for any population since there is insufficient evidence comparing it to the recommended, initial therapies. EIs: No head-to-head trials were identified to directly compare the approved entry inhibitors. The DHHS guidelines reserve recommending the entry inhibitors for initial therapy; however, of the two, maraviroc’s labeling does not restrict its use to treatment-experienced patients as is the case for enfuvirtide. Both entry inhibitors are approved for use in the pediatric population, with maraviroc carrying approval for younger children. Maraviroc is administered orally, whereas enfuvirtide is administered via subcutaneous injection. Maraviroc, unlike enfuvirtide, undergoes metabolism via Cytochrome P450, posing a greater potential for drug interactions. 5 Introduction The present day human immunodeficiency virus type-1 (HIV-1) disease state is a chronic plight, challenged by the emergence of therapy-resistant strains, opportunistic infections, and medication complexities. Incidence in the United States is dominated by the HIV-1 subtype, whereas HIV-2 is most prevalent in West Africa.1 Transmission of HIV can occur through exposure to infected blood, reproductive fluids, and breast milk.2 Once infected, the HIV-1 disease path may vary between individuals. Generally the disease follows a multiphasic progression, where the primary infection event is often followed by acute HIV dissemination syndrome and then enters clinical latency.2 Severe damage to the host’s immune system may progress as virulence of the virus augments through rapid mutations conferring resistance to medications. Without an effective therapeutic regimen, the patient is burdened by constitutional symptoms and illness from opportunistic infections leading to the end-of-life. In order to limit failure from viral resistance, an approach termed “highly active antiretroviral therapy” is implemented, combining three agents from at least two different drug classes— the standard of care in first-line HIV-1 therapy.3 The multidrug regimen is tailored to the patient’s comorbidities and concurrent medications, with the goal of therapy to preserve and improve immunologic function, and ideally suppress the plasma viral ribonucleic acid (RNA) load below detectable levels (HIV RNA< 20 to 75 copies/mL, assay dependent). The precise cut-off used to define virological failure remains an area of debate and study. The guidelines by the Department of Health and Human Services (DHHS) and the AIDS Clinical Trials Group currently define virological failure as an HIV RNA load >200 copies/mL.3 The HIV-antiretroviral drug armada includes the nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors (PIs), entry inhibitors (EIs), integrase strand-transfer inhibitors (INSTIs), and two pharmacokinetic enhancers. Table 1 of Appendix A displays the currently available antiretroviral agents indicated/labeled for the treatment of HIV-1. This review will evaluate the safety and efficacy of the single-active-ingredient containing products among the INSTI, NNRTI, and EI drug classes for the treatment of HIV-1. The single-ingredient elvitegravir product, Vitekta®, was voluntarily removed from the market in February 2017 due to low utilization.4 It remains available in combination products as Genvoya® and Stribild®. Within these three drug classes, efavirenz, rilpivirine, and dolutegravir are also available in complete-regimen combination products. Combination products will be compared in a review separate from this document and presented in April. Table 1 provides a summary of the dosage forms and approved dosing for the single-ingredient products included in this review. The NNRTIs and the EI, enfuvirtide, are neither indicated nor effective for HIV-2 treatment. The INSTIs and the EI, maraviroc, may have activity against HIV-2, however, are not approved by the Federal Drug Administration (FDA) for this indication.3 Treatment of HIV-2 will not be a focus of this review and discussion will be referring to HIV-1 treatment hereinafter. 6 Table 1. Single-Ingredient INSTI, NNRTI, and EI Products FDA-Approved for the Treatment of HIV-1 5-16 Brand Name/Dosage Forms Indication/Dose (generic available if italicized) Integrase Strand Transfer Inhibitors No generic available Labeled Indication: Treatment of HIV-1 in combination ARV therapy for treatment-naïve and experienced adults and children Dolutegravir Tivicay®: Adult Dose: DTG • 10mg tablet • 50mg QD; Increase to BID dosing when taken with UGT1A or CYP3A inducers, or with certain INSTI-resistant strains • 25mg tablet Pediatric Dose: for pediatric patients at least 30kg • 50mg tablet • If at least 40kg: dosed as 50mg QD • For 30kg to less than 40kg: dosed as 35mg QD • Increase frequency to BID with certain UGT1A or CYP3A inducers and with certain INSTI-associated resistance substitutions No generic available Labeled Indication: Treatment of HIV-1 in combination ARV therapy for treatment-naïve and treatment-experienced patients 4-weeks or older Raltegravir Isentress®: RAL • 25mg chewable tablet Adult Dose: • 100mg chewable tablet • 400 mg tablet BID • 100 mg/5mL oral suspension • During co-administration with rifampin, increase to 800 mg BID. • 400mg tablet Pediatric Dose: • If at least 25kg: One 400mg tablet BID • If at least 11kg: Chewable tablets dosed between 75mg and 300mg BID based on weight • If at least 3 kg to less than 25 kg: Oral suspension dosed between 20mg and 100mg BID based on weight. 7 Brand Name/Dosage Forms Indication/Dose (generic available if italicized) Non-Nucleoside Reverse Transcriptase Inhibitors No generic available Labeled Indication: Treatment of HIV-1 in combination with other ARV agents for patients as least 16 years old. Package insert note: It is important to consider that there is insufficient data directly comparing delavirdine-based regimens Delavirdine Rescriptor®: with currently preferred 3-drug regimens for initial treatment of HIV. DLV • 100mg dispersible tablet • 200mg tablet • Treatment guidelines no longer recommended this drug for treatment- naïve patients Dose: 400mg TID No generic available Labeled Indication: Treatment of HIV-1 in combined ARV therapy for adults and pediatric patients at least 3 months old and weighing at least 3.5 kg Efavirenz Sustiva®: EFV • 50mg capsule Adult Dose: • 200mg capsule • 600mg QD on an empty stomach preferably at bedtime to limit CNS side effects • 600mg tablet Pediatric Dose: at least 3 months old and weighing at least 3.5kg • Sprinkle capsule in food; dosed between 100mg and 600mg QD, based on weight No generic available Labeled Indication Treatment of HIV-1 in combination ARV therapy for treatment-experienced patients 6 years or older with documented viral resistance to other NNRTI and ARV agents Etravirine Intelence®: Dispersible tablets ETR • 25mg tablet Adult Dose: • 100mg tablet • 200mg BID following a meal • 200 mg tablet Pediatric Dose: for age 6 up to 18 years old weighing at least 16kg • May disperse tablet in water; dosed between 100mg and 200mg BID, based on weight Generics available Labeled Indication: Treatment of HIV-1 in combined ARV therapy for patients at least 15 days old •Must have CD4-count >250cells/mm3 for females and >400 cells/mm3 for males Viramune®: • A 14-day lead-in dosing should be carried out to reduce the risk of rash Nevirapine • 200 mg tablet NVP Dose: for patients at least 16 years old • 50mg/5mL oral • IR-tablet: 200mg QD x 14 days for lead-in period, then 200mg BID thereafter suspension • ER-tablet: 400mg QD for maintenance therapy Viramune XR: • 100mg tablet Pediatric Dose: for patients at least 15 days old • 400mg tablet • IR-tablet: 150mg/m2 QD x 14 days followed by 150mg/m2 BID thereafter, not to exceed 400mg per day • ER-tablet dosed between 200mg and 400mg QD based on body surface area Black Box Warning Key Concerns: Hepatotoxicity; Life-threatening skin reactions No generic available Labeled Indication: Treatment of HIV-1 in combination ARV therapy for treatment-naive patients at least 12 years old, Rilpivirine weighing at least 35kg, and with HIV-1 RNA ≤100,000 copies/mL at baseline RPV Edurant®: • 25mg tablet Dose: 25mg QD with a meal 8 Brand Name/Dosage Forms Indication/Dose (generic available if italicized) Entry Inhibitors No generic available Labeled Indication: Treatment of HIV-1 in combination ARV therapy for treatment-experienced patients 6 years or older Enfuvirtide Fuzeon®: Dose: ENF • 90mg/mL • 90mg (1mL) injected subcutaneously BID SQ-solution Pediatric Dose: for patients 6 to 16 years old • 2mg/kg subcutaneously BID, up to a maximum dose of 90mg BID No generic available Labeled Indication: Treatment of HIV-1 in combined ARV therapy for adults and pediatric patients at least 2 years old. Prior to initiation patients must be tested for CCR5 tropism using a highly sensitive assay. Maraviroc Selzentry®: MVC • 150mg tablet Adult Dose • 300mg tablet’ • Dosed between 150mg and 600mg BID, depending on concomitant medications that the affect CYP3A4 Anticipated formulations: Pediatric Dose: for patients weighing at least 10kg 25mg tablet, 75mg tablet, and • Dosed between 50mg and 300mg BID, depending on weight and concomitant medications 20mg/mL oral solution15 Abbreviation key: ARV- antiretroviral, BID- twice daily, DVL- delavirdine, DTG-dolutegravir, EFV- efavirenz, ENF- enfuvirtide, ER- extended release, ETR- etravirine, EVG- elvitegravir, IR- immediate release, INSTI- integrase strand transfer inhibitor, MVC- maraviroc, NNRTI- non-nucleotide reverse transcriptase inhibitor, NVP-nevirapine, QD- once daily, RAL- raltegravir, RPV- rilpivirine, TID- three times daily 9 Disease Overview Epidemiology Although the nation’s annual rate of newly-diagnosed HIV cases declined by 19% from 2005 to 2014, the disease continues to affect more than 1.2 million people in the United States.17 Groups at highest risk of becoming infected include men who have sex with men, IV- drug users, African Americans, Hispanics, and Latinos.17 The rate of newly-diagnosed cases in Utah during 2015 was 4 per 100,000 populations (108 males and 12 females) and has fluctuated between 3.3 and 5 per 100,000 populations over the last ten years.18,19 Data from 2013 last cited the prevalence of HIV cases in Utah to be 2,565 persons.20 Considering the trend of an increasing male incidence rate in Utah, especially in the 35 and younger category (composing 53% of the newly-diagnosed male cases in 2015), the Utah Department of Health (UDH) has advocated targeting young men for HIV testing.18,21 In contrast, the incidence among females has remained steady and is more evenly distributed across age groups in Utah.18 With regard to children, nine newly-diagnosed cases were reported in Utah between 2005 and 2014 in the 13 and younger age group.19 Tracking and establishing a linkage-to-care goal upon a positive diagnosis is of particular importance considering the context of recently published guidelines highlighting evidence supporting prompt antiretroviral (ARV) therapy initiation for all infected individuals, with rare exceptions, regardless of the CD4 T lymphocyte (CD4) count.3,17,22 The UDH strives to have newly infected patients linked to care within three months. In 2015, 67% of newly diagnosed patients in Utah obtained care within a month of diagnosis, and by three months 88% were considered linked to care.23 Further background information concerning the timing of antiretroviral therapy (ART) initiation is outlined in Table 2 of Appendix A. HIV-1 Treatment Pharmacotherapy strategies target pivotal enzymes or receptors involved in the HIV infection cycle —fusion and entry into the host cell (via glycoprotein (gp) 41 and C-C chemokine type 5 receptor (CCR5)), conversion of HIV RNA into double-stranded deoxyribonucleic acid (DNA) (via reverse transcriptase), integration of viral-coded DNA into the host’s genome (via integrase), and cleavage of gag-pol polyprotein for viral maturation (via protease).24 Once integrated into the host’s genome, HIV causes a deficiency of helper T lymphocytes and a profound immunodeficiency.2 Consideration of both the extent of immunosuppression and the current presenting symptoms are important when deciding prophylactic treatment.3 When the CD4 count falls below 500 cells/µL, patients are at a high risk of developing opportunistic infections (OIs) including, but not limited to, P. jiroveci, Mycobacterium, and Cytomegalovirus. Prior to treatment, genotypic resistance testing is performed to guide medication selection. Patients are also screened for tuberculosis and hepatitis B and C viruses. A positive diagnosis will influence the selection of the appropriate ARV regimen. Other pre-treatment tests include a co-receptor tropism assay prior to maraviroc initiation and HLA-B*5701 screening to assess abacavir-hypersensitivity risk. Two surrogate markers, CD4-lymphocyte count and plasma HIV RNA, are used to assess the patient’s response to therapy and guide opportunistic prophylaxis. When treatment is expedited before resistance results are available, the NNRTI- based regimens should be avoided; pre-existing resistance to INSTIs and PI-based regimens is less likely and serve as better options in this situation.3 The guidelines published by the DHHS and the International Antiviral Society-USA Panel (IAS-USA), for the management of HIV infection in the United States, are congruent to one 10
Description: