K/DOQI Clinical Practice Guidelines for Bone Metabolism and Disease in Children With Chronic ... PDF
Preview K/DOQI Clinical Practice Guidelines for Bone Metabolism and Disease in Children With Chronic ...
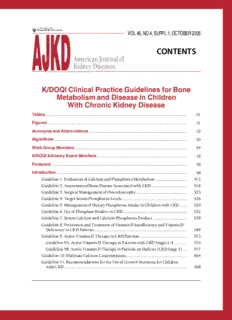
AJKD VOL46,NO4,SUPPL1,OCTOBER2005 CONTENTS AmericanJournalof KidneyDiseases K/DOQI Clinical Practice Guidelines for Bone Metabolism and Disease in Children With Chronic Kidney Disease Tables............................................................................................................................... S1 Figures............................................................................................................................. S1 AcronymsandAbbreviations........................................................................................ S2 Algorithms....................................................................................................................... S3 WorkGroupMembers..................................................................................................... S4 K/DOQIAdvisoryBoardMembers................................................................................. S5 Foreword.......................................................................................................................... S6 Introduction..................................................................................................................... S8 Guideline1.EvaluationofCalciumandPhosphorusMetabolism............................ S12 Guideline2.AssessmentofBoneDiseaseAssociatedwithCKD................................ S18 Guideline3.SurgicalManagementofOsteodystrophy............................................. S23 Guideline4.TargetSerumPhosphorusLevels.......................................................... S26 Guideline5.ManagementofDietaryPhosphorusIntakeinChildrenwithCKD...... S29 Guideline6.UseofPhosphateBindersinCKD......................................................... S32 Guideline7.SerumCalciumandCalcium-PhosphorusProduct.............................. S39 Guideline8.PreventionandTreatmentofVitaminDInsufficiencyandVitaminD DeficiencyinCKDPatients................................................................................... S48 Guideline9.ActiveVitaminDTherapyinCKDPatients.......................................... S53 Guideline9A.ActiveVitaminDTherapyinPatientswithCKDStages2-4........... S53 Guideline9B.ActiveVitaminDTherapyinPatientsonDialysis(CKDStage5)... S57 Guideline10.DialysateCalciumConcentrations...................................................... S64 Guideline11.RecommendationsfortheUseofGrowthHormoneforChildren withCKD.............................................................................................................. S68 Guideline12.AluminumOverloadandToxicityinCKD.......................................... S70 Guideline13.TreatmentofAluminumToxicity....................................................... S79 Guideline14.TreatmentofBoneDiseaseinCKD..................................................... S87 Guideline14A.Hyperparathyroid(High-Turnover)BoneDisease....................... S87 Guideline14B.Rickets/Osteomalacia.................................................................... S87 Guideline14C.AdynamicBoneDisease................................................................ S88 Guideline15.ParathyroidectomyinPatientswithCKD........................................... S91 Guideline16.MetabolicAcidosis.............................................................................. S94 Guideline17.BoneDiseaseinthePediatricKidneyTransplantRecipient................ S96 Afterword......................................................................................................................... S99 BiographicalSketchesofWorkGroupMembers........................................................ S101 References....................................................................................................................... S103 Tables Table1. SignsandSymptomsofBoneDiseaseinChildrenwithCKD..........................................S9 Table2. FrequencyofMeasurementofPTH,Calcium,Phosphorus,TotalCO ,and 2 AlkalinePhosphatasebyStageofCKD...........................................................................S12 Table3. TargetRangeofSerumPTHbyStageofCKD................................................................S12 Table4. HistologicalFeaturesofHigh-TurnoverRenalOsteodystrophy......................................S19 Table5. HistologicalFeaturesofLow-TurnoverRenalOsteodystrophy......................................S19 Table6. RepresentativeNormalValuesforSerumPhosphorus,TotalCalcium,Blood IonizedCalcium,andAlkalinePhosphataseConcentrations...........................................S26 Table7. DietaryReferenceIntakesofPhosphorusinChildren.....................................................S29 Table8. StepstoCalculatetheInitialBinderPrescription............................................................S33 Table9. Phosphorus-BindingCompounds....................................................................................S33 Table10. RecommendationsforCalciumIntake............................................................................S40 Table11. CalciumContentofCommonCalcium-BasedBinders...................................................S41 Table12. Low-Phosphorus,High-CalciumFoods..........................................................................S42 Table13. PartialListofCalcium-ContainingSupplements............................................................S43 Table14. DeterminingCalciumRequirementsinAdultsAged19-30Years..................................S45 Table15. RecommendedSupplementationforVitaminDDeficiency/Insufficiencyin PatientswithCKDStages3-4.........................................................................................S48 Table16. SerumLevelsofPTH,Calcium,andPhosphateRequiredforInitiationofOral VitaminDSterolTherapy,andRecommendedInitialDosesinPatientswith CKDStages2-4...............................................................................................................S53 Table17. InitialCalcitriolDosingRecommendationsforChildrenonMaintenanceDialysis.......S57 Table18. Aluminum-RelatedDisorders:Features,Causes,andConsiderationsforTherapy........S71 Table19. FrequencyforMeasurementofSerumLevelsofTotalCO ...........................................S94 2 Table20. FrequencyofMeasurementofCalcium,Phosphorus,PTH,andTotalCO after 2 KidneyTransplantation....................................................................................................S96 Figures Figure1. RelationshipbetweenSerumiPTHLevelsandCCR.........................................................S13 Figure2. SummaryROCAnalysisofErosionsonX-RayasDiagnosticforOsteitisFibrosa..........S14 Figure3. SummaryROCAnalysisofIntactPTHforDiagnosisofHigh-TurnoverBoneDisease...S15 Figure4. SummaryROCAnalysisofIntactPTHforDiagnosisofLow-TurnoverBoneDisease...S16 Figure5. Meta-AnalysisofSizeofEffectonSerumPhosphorusLevelsofCalcium AcetateversusCalciumCarbonate....................................................................................S35 Figure6. Meta-AnalysisofSizeofHypercalcemicEffectofCalciumCarbonateversus OtherPhosphateBinders....................................................................................................S35 Figure7. Meta-AnalysisofOralversusIntravenousCalcitriolonPTHSuppression.......................S62 Figure8. IndividualStudyandSummaryEffectsizesfortheEffectofDFOTherapy onBoneFormationRate....................................................................................................S83 Figure9. IndividualStudyandSummaryEffectSizesfortheEffectofDFOTherapyon BoneSurfaceAluminumStain...........................................................................................S83 AmericanJournalofKidneyDiseases,Vol46,No4,Suppl1(October),2005:pS1 S1 Acronyms andAbbreviations 1stPTH-IMA First-generationparathyroidhormoneimmunometricassay 2°HPT Secondaryhyperparathyroidism AIs Adequateintakes AVN Avascularnecrosis BCG Bromocresolgreenmethod BFR Boneformationrate BMC Bonemineralcontent BMD Bonemineraldensity CaR Calcium-sensingreceptors CAPD Continuousambulatoryperitonealdialysis CaXP Calcium-phosphorusproduct CCR Creatinineclearancerate CKD Chronickidneydisease CRF Chronicrenalfailure DBP VitaminD-bindingprotein DEXA DualenergyX-rayabsorptiometry DFO Desferrioxamine DOQI DialysisOutcomesQualityInitiative DRI DietaryReferenceIntake EBCT Electronbeamcomputedtomography EEG Electroencephalogram ESRD End-stagerenaldisease GFR Glomerularfiltrationrate GH,rhGH Growthhormone,recombinanthumangrowthhormone ICMA Immunochemiluminometricassay IGF Insulin-likegrowthfactor IRMA Immunoradiometricassay K/DOQI KidneyDiseaseOutcomesQualityInitiative MCV Meancellvolume MDRD ModificationofDietinRenalDisease MRI Magneticresonanceimaging NKF NationalKidneyFoundation PBM Peakbonemass PTH Parathyroidhormone QCT Quantitativecomputedtomography RDA Recommendeddietaryallowance RDI Recommendeddailyintake ROC Receiveroperatingcharacteristics SCFE Symptomaticproximalfemoralslippedepiphyses SD Standarddeviation VDR VitaminDreceptor VDRE VitaminDreceptorelement,vitaminD-responsiveelement S2 AmericanJournalofKidneyDiseases,Vol46,No4,Suppl1(October),2005:pS2 Algorithms Algorithm1. VitaminDSupplementationinCKD(Stages2-4)..................................................................................S49 Algorithm2. ManagementofCKDPatients(Stages2-4)withActiveVitaminDSterols...........................................S54 Algorithm3. ManagingVitaminDSterolsBasedonSerumCalciumLevels..............................................................S59 Algorithm4. ManagingVitaminDSterolsBasedonSerumPhosphorusLevels........................................................S60 Algorithm5. ManagingVitaminDSterolsBasedonPTHLevelsinChildrenNot ReceivingGrowthHormones.................................................................................................................S61 Algorithm6. EvaluationofAluminumNeurotoxicity..................................................................................................S72 Algorithm7. EvaluationofAluminum-RelatedDisorders:ConsiderationsforDFOTest andSubsequentDFOTreatment.............................................................................................................S73 Algorithm8. DFOTreatmentAfterP Risebetween50-300(cid:1)g/L............................................................................S80 Al Algorithm9. SubsequentDFOTreatmentafterP Rise(cid:2)300(cid:1)g/L..........................................................................S81 Al AmericanJournalofKidneyDiseases,Vol46,No4,Suppl1(October),2005:pS3 S3 K/DOQI Clinical Practice Guidelines for Bone Metabolism and Disease in Children with Chronic Kidney Disease Work Group Membership WorkGroupCo-Chairs CraigB.Langman,MD IsidroB.Salusky,MD NorthwesternUniversityFeinbergSchoolofMedicine DavidGeffenSchoolofMedicineatUCLA Children’sMemorialHospital LosAngeles,CA Chicago,IL WorkGroup LarryGreenbaum,MD,PhD PaulineNelson,RD MedicalCollegeofWisconsin UCLAMedicalCenter Milwaukee,WI LosAngeles,CA HaraldJueppner,MD AnthonyPortale,MD MassachusettsGeneralHospital UniversityofCaliforniaSanFrancisco HarvardMedicalSchool SanFrancisco,CA Boston,MA BradleyA.Warady,MD MaryLeonard,MD TheChildren’sMercyHospital Children’sHospitalofPhiladelphia KansasCity,MO Philadelphia,PA ConsultantstotheWorkGroup RichardE.Bowen,MD WilliamL.Oppenheim,MD AssistantClinicalProfessor DavidGeffenSchoolofMedicineatUCLA DavidGeffenSchoolofMedicineatUCLA LosAngeles,CA LosAngeles,CA K/DOQIAdvisory Board Members AdeeraLevin,MD,FACP K/DOQIChair MichaelRocco,MD,MS K/DOQIVice-Chair GarabedEknoyan,MD NathanLevin,MD,FACP K/DOQICo-ChairEmeritus K/DOQICo-ChairEmeritus GeorgeBailie,PharmD,PhD WilliamMitch,MD BryanBecker,MD JosephV.Nally,MD PeterG.Blake,MD,FRCPC,MBB.Ch GregorioObrador,MD,MPH AllanCollins,MD,FACP RulanS.Parekh,MD,MS PeterW.Crooks,MD ThakorG.Patel,MD,MACP WilliamE.Haley,MD BrianJ.G.Pereira,MD,DM AlanR.Hull,MD NeilR.Powe,MD LawrenceHunsicker,MD ClaudioRonco,MD BertrandL.Jaber,MD AntonC.Schoolwerth,MD CyndaAnnJohnson,MD,MBA RaymondVanholder,MD,PhD GeorgeA.Kaysen,MD,PhD NanetteKassWenger,MD KarrenKing,MSW,ACSW,LCSW DavidWheeler,MD,MRCP MichaelKlag,MD,MPH WinfredW.Williams,Jr.,MD CraigB.Langman,MD Shuin-LinYang,MD DerrickLatos,MD DonnaMapes,DNSc,MS Ex-Officio LindaMcCann,RD,LD,CSR JosephineBriggs,MD RavindraL.Mehta,MD,FACP DavidWarnock,MD MaureenMichael,BSN,MBA K/DOQI Guideline Development NKF Staff DonnaFingerhut LoriMormino MargaretFiorarancio KerryWillis,PhD AnthonyGucciardo AJKD VOL46,NO4,SUPPL1,OCTOBER2005 AmericanJournalof KidneyDiseases Foreword T HE DISCIPLINE OF pediatric nephrol- disease associated with calcium in incorrect ogy is unique and challenging because it places within the vasculature, similar to that encompasses the widest developmental stages seen in adult patients who develop CKD de of life, from in utero presentation of chronic novo. We recognize the pervasive nature of kidney disease (CKD) through kidney failure CKD,andperhapsamoresubtlemanifestation presenting in early adulthood. CKD in our of its osteodystrophy, in abnormal neurologi- patients may arise from embryological distur- caldevelopmentofouryoungestpatients. bances, genetic mutations, acquired glomeru- Although we were members of the commit- lopathiesand/ortubulopathies,systemicmeta- tee for the preparation and publication of the bolic diseases, immune-mediated diseases, or National Kidney Foundation K/DOQI Guide- thosediseasesthatderive—inpart—fromlife- linesforbonemetabolismanddiseaseinCKD style choices. The natural history of many of inadults,werecognizedthatthesubjectinthat these diseases is being rewritten continually, population was filled with enough controversy as longevity for patients increases beyond that that recommendations for children could not seen by our mentors before us. We see the properly be placed within it. Therefore, the influence of socio-demographic distributions leaders of the K/DOQI process acceded to our on disease expression and severity, and the request for a meeting in Chicago, in October insufficiencies of organ availability for trans- 2002, to begin the arduous process of sorting plantationondiseasechronicity. through the literature to produce a pediatric- In the pediatric population, body calcium specific set of K/DOQI guidelines for bone balance remains markedly positive to support metabolism and disease in CKD with our col- both somatic growth and bone mineral accre- leaguesandcommitteemembers. tion.The sine qua non of pediatric CKD is the The task differed initially from the resultant marked change in these two processes that guidelines seen here; but with very limited leadstothedevastatingclinicaldiseasethatwe resources, and no external review of extant term “osteodystrophy.” We have come to real- literature by a third party, we decided late in ize that the disorder encompasses marked dis- 2003 to follow the structure of the adult-based turbancesinmineralhomeostasiswithchronic bone metabolism and disease guidelines in- metabolic acidosis, secondary hyperparathy- stead. We owe great thanks to that group for roidism (2° HPT), insufficiency of 1,25-dihy- their wisdom in allowing us to use some of droxyvitaminD,andfailureoflineargrowthin theirwork,andadaptitwhereindicatedforthe addition to extraskeletal disease. Thus, we aspects unique to pediatric osteodystrophy. It have seen children, adolescents, and young became rather clear, quickly, that the area of adults with an as yet undefined cardiovascular osteodystrophy in pediatric CKD is highly uninvestigated, and is a wonderful career- buildingopportunityforthegenerationofpedi- ©2005bytheNationalKidneyFoundation,Inc. atric nephrologists who will follow the mem- 0272-6386/05/4604-0101$30.00/0 doi:10.1053/j.ajkd.2005.07.024 bersofthiswritingcommittee. S6 AmericanJournalofKidneyDiseases,Vol46,No4,Suppl1(October),2005:ppS6-S7 FOREWORD S7 AsCo-Chairs,weoweadeepgratitudetoour and Adeera Levin are to be commended for committee members. Each worked long hours, their spiritual input to our project (and our- acceded to our many requests on short notice selves)duringitslongcourse. with a ‘can-do’attitude, and worked in a colle- As you, the Reader, use these guidelines, you gial manner that allowed the project to succeed willbequicktoseeitsflawsandweaknesses,asall inaloftymanner. such guidelines possess. We welcome your input With the successful completion of our task, directlythroughtheNationalKidneyFoundationto thoseareasthatneedimprovement,emendation,or we need to thank many of our colleagues who removal in subsequent iterations of the work. De- didnotserveonthecommittee,butwhotaught spitethiscaveat,webelievethatregularattentionto us much from their science, and from their our patients’ osteodystrophy in a manner pro- empathetic care of patients. We hope we ac- scribed within the guidelines will lead to an im- knowledged, by attribution within our text, provedoutcomeineveryfacetofthedisease. their work and toil, and we take responsibility foranymistakesofomissioninthisregard.We thank the entire staff of the National Kidney Foundation for their excellent support, and CraigB.Langman,MD especially that of Mr.Anthony Gucciardo and WorkGroupCo-Chair Ms. Donna Fingerhut, who were tireless in IsidroB.Salusky,MD their pursuit of our goals. Drs. Gary Eknoyan WorkGroupCo-Chair Introduction GROWTH AND DEVELOPMENT andelaborationofmatrixresultinlineargrowth. OF THE SKELETON Ossificationproceedstowardtheendofthebone During childhood and adolescence, total and ultimately forms the growth plate (epiphy- skeletalcalciumincreasesfromapproxi- seal plate or physis) that is the predominant site mately25gatbirthto900gand1,200ginadult of longitudinal bone growth. With continued females and males, respectively. Attainment of maturation,thegrowthplatethinsandeventually optimal peak bone mass by young adulthood is disappears with fusion of the epiphyseal and thoughttobethebestprotectionagainstosteopo- diaphysealossificationcenters.Epiphysealunion rosis later in life.1 Therefore, childhood and occurs at an earlier age in females than males. adolescence are particularly critical periods for Knowledgeabouttheappearanceofvariousossi- theestablishmentoflife-longbonehealth.While fication centers in the carpal bones is used to peakbonemassisstronglyinfluencedbygenetic determine a child’s maturational age, or “bone factors, full genetic potential is attained only if age.” nutrition, growth, physical activity, and meta- bolicandendocrinefunctionareoptimalinchil- BONE MODELING dren.The clinical features of renal bone disease Theshapeandstructureofbonesarecontinu- unique to childhood relate to distinctions be- ously modified and renovated by two different tweenthegrowingandthefully-grownskeleton. processesduringgrowth:modelingandremodel- The metabolic process of skeletal modeling ing. Both processes result in the replacement of throughout growth dictates that pediatric-spe- old bone tissue with new bone. The remodeling cific recommendations for the management of cycle of bone resorption and formation takes thebonediseaseofCKDbedeveloped. place throughout life and is vital for microdam- age repair and maintenance of skeletal integrity. Incontrast,modelingpredominatesduringgrowth BONE FORMATION andpromotesformationofnewboneatlocations Formation of the skeleton occurs by two pro- different from the sites of bone resorption. This cessesofossification—intramembranousanden- results in increased bone mass and modification dochondral. Intramembranous ossification is the ofboneshape.Forexample,increasesincortical direct mineralization of vascular connective tis- bonediameterofthediaphysisareduetoconcur- sue membrane in the plate-like bones of the rent bone formation on the periosteal (outer) skull, facial bones, mandible, and clavicle. The surface and bone resorption on the endosteal transformationofmesenchymalcellsintoosteo- (inner)surface.Incontrast,asthebonegrowsin blasts and production of osteoid matrix convert length,thewidemetaphysealregionisconverted theprimitivemesenchymeintobone.Incontrast, to a narrow diaphysis through resorption of the bones that involve joints and bear weight form periosteal surface and bone formation on the byendochondralossification.Endochondralbone endosteal surface. Finally, long bones drift in a formationistheresultofossificationofaninter- lateral direction during growth due to relatively mediate cartilage model that is derived from greater resorption along the medial edge of the mesenchyme and represents the position and boneandformationalongthelateraledge. shape of the bone to be formed at that site.This In conclusion, bone growth during childhood providesamechanismfortheformationofbone andadolescenceinvolvesthecomplexcoordina- duringgrowth.Inthelongbonesoftheextremi- tion of varied cell activities on specific bone ties, the primary center of ossification is located surfaces.Cartilageproliferation,bonemodeling, in the central portion of the cartilage model. andepiphysealclosureareunderthedirectinflu- Proliferation and hypertrophy of chondrocytes ence of a variety of hormones and growth fac- tors, such as growth hormone (GH), thyroid hormone,estrogen,testosterone,parathyroidhor- ©2005bytheNationalKidneyFoundation,Inc. mone(PTH),vitaminD,andinsulin-likegrowth 0272-6386/05/4604-0102$30.00/0 doi:10.1053/j.ajkd.2005.07.025 factors (IGF).2 Each of these factors may be S8 AmericanJournalofKidneyDiseases,Vol46,No4,Suppl1(October),2005:ppS8-S11
Description: