Children's Healthy Living (CHL) PDF
Preview Children's Healthy Living (CHL)
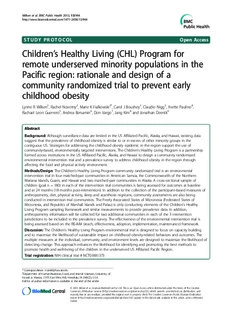
Wilkenetal.BMCPublicHealth2013,13:944 http://www.biomedcentral.com/1471-2458/13/944 STUDY PROTOCOL Open Access ’ Children s Healthy Living (CHL) Program for remote underserved minority populations in the Pacific region: rationale and design of a community randomized trial to prevent early childhood obesity Lynne R Wilken1, Rachel Novotny2, Marie K Fialkowski2*, Carol J Boushey1, Claudio Nigg3, Yvette Paulino4, Rachael Leon Guerrero5, Andrea Bersamin6, Don Vargo7, Jang Kim8 and Jonathan Deenik9 Abstract Background: Although surveillance data are limited in the US Affiliated Pacific, Alaska, and Hawaii, existing data suggest thatthe prevalence of childhood obesity is similar to or inexcessof other minority groups inthe contiguous US. Strategies for addressing thechildhood obesity epidemic inthe region support theuse of community-based,environmentally targeted interventions. The Children’sHealthy Living Program is a partnership formed across institutions in theUS AffiliatedPacific,Alaska, and Hawaii to design a communityrandomized environmental interventiontrial and a prevalence survey to address childhood obesity in theregionthrough affecting the food and physical activity environment. Methods/Design:The Children’sHealthy Living Program community randomized trial is an environmental intervention trial in four matched-pair communities inAmerican Samoa, the Commonwealth of theNorthern Mariana Islands, Guam, and Hawaii and two matched-pair communities in Alaska. A cross-sectionalsampleof children (goal n =180) in each of theintervention trial communitiesis being assessed for outcomesatbaseline and at24 months (18 months post-intervention). Inaddition to the collection ofthe participant-based measures of anthropometry,diet, physical activity, sleep and acanthosis nigricans, community assessments are also being conducted ininterventiontrial communities. The Freely Associated States of Micronesia (Federated States of Micronesia, and Republics ofMarshall Islands and Palau) is only conducting elements of theChildren’sHealthy Living Program sampling framework and similar measurements to provide prevalence data.Inaddition, anthropometry informationwill be collected for two additional communities ineach of the5 intervention jurisdictions to be included in theprevalencesurvey. The effectiveness oftheenvironmentalinterventiontrial is being assessed based onthe RE-AIM (reach, effectiveness, adoption, implementation, maintenance) framework. Discussion: The Children’s Healthy Living Program environmentaltrial is designed to focus on capacity building and to maximize thelikelihood of sustainable impact on childhood obesity-related behaviors and outcomes. The multiple measures atthe individual, community, and environment levels are designed to maximize the likelihood of detecting change. This approach enhances thelikelihood for identifying and promoting the best methods to promote health and well-beingof the children inthe underserved US Affiliated Pacific Region. Trial registration: NIH clinical trial # NCT01881373 *Correspondence:[email protected] 2DepartmentofHumanNutrition,Food,andAnimalSciences,Universityof HawaiiatManoa,(1955East-WestRd),Honolulu,HI(96822),USA Fulllistofauthorinformationisavailableattheendofthearticle ©2013Wilkenetal.;licenseeBioMedCentralLtd.ThisisanOpenAccessarticledistributedunderthetermsoftheCreative CommonsAttributionLicense(http://creativecommons.org/licenses/by/2.0),whichpermitsunrestricteduse,distribution,and reproductioninanymedium,providedtheoriginalworkisproperlycited.TheCreativeCommonsPublicDomainDedication waiver(http://creativecommons.org/publicdomain/zero/1.0/)appliestothedatamadeavailableinthisarticle,unlessotherwise stated. Wilkenetal.BMCPublicHealth2013,13:944 Page2of13 http://www.biomedcentral.com/1471-2458/13/944 Background olds) in Guam, using US CDC reference data [18]. Al- Epidemiologyofchildobesity though these estimates are informative, it is important Global prevalence estimates indicate that in 2004 ap- to note that data are derived from small samples and proximately 10% (150-160 million) of school-aged chil- maynotberepresentative ofthepopulation. dren (5 to 17 years) were overweight, and 2-3% (35-40 Overweight and obese combined (≥85th percentile million) were obese [1]. In the United States (US), the BMI-for-age) prevalence estimates from NHANES in prevalence of obesity alone was estimated at 17% among 2007-2008 [19], among 2-5 year olds, are 21.2% overall 5 to 19 year-olds in 2009-2010 [2]. However, adequate and 26.0%, 27.7%, and 27.7% for the minority popula- prevalence data are lacking on overweight and obesity in tionsofnon-Hispanicblack,totalHispanic,andMexican thePacific Region. American children, respectively. Among 6-11 year olds The health and social consequences of excess weight from NHANES in 2007-2008 overweight and obese are substantial, and obese and overweight children are at combined (≥85th percentile BMI-for-age) prevalence es- risk for serious chronic illnesses. For example, being timates are 35.5% overall and 37.6%, 42.6%, and 41.7% overweight and obese is a major risk factor for type 2 for theminoritypopulations ofnon-Hispanic black,total diabetes in children [3,4]. Obese children are also more Hispanic, and Mexican American children, respectively. likely than their peers to experience negative social and The 2009-2010 cycle of NHANES documents similarly psychological consequences including discrimination, highprevalenceamongsomeUSminority groups(Black, stigmatization,andlowself-esteem [5-8]. Mexican American) [2]. These estimates are similar to Most researchers use body mass index (BMI) to meas- the existing estimates from the noncontiguous US states ure child overweight and obesity; however, the BMI and US Affiliated Pacific Island Jurisdictions. Data from levels defining overweight and obesity may differ across the Supplemental Nutrition Program for Women, In- countries depending on the reference data and cutpoints fants and Children (WIC) in 2006 estimate prevalenceof used [9]. Global estimates are often based on the World combined overweight and obesity (≥85th percentile BMI- Health Organization cutpoints, which define overweight for-age) in children ages 2-5 years at 34.7% for Native as > 1SD and obesity as > 2SD above the average (M) American/Alaska Native and 33.4% for Native Hawaiian/ where M and SD are derived from a reference popula- Pacific Islanders [20]. In contrast, the estimates among tion for 5 to 19 year-olds, using data sets compiled by the Asian, Black, and White children are 17.9%, 20.8%, WHO [10,11]. In the US, in children aged 2 to 19 years, and21.5%,respectively [20]. overweight is usually defined as greater than or equal to Despite the serious underrepresentation of the Pacific the 85th percentile but less than the 95th percentile and Region in obesity research, the high prevalence of obesity as greater than or equal to the 95th percentile, chronic conditions in the region has prompted the US according to the BMI-for-age Centers for Disease Affiliated Pacific Islands (AS, CNMI, Guam, FSM, Palau Control andPrevention (CDC)growthcharts[12]. and RMI) to declare a “State of Emergency” [21]. Evidenced by the high proportions of Pacific Island PrevalenceofobesityintheUSaffiliatedpacificregion adults who are overweight and obese, prevention of Data from the National Health and Nutrition Examin- overweight and obesity among children in the Pacific as ation Survey (NHANES), a program of studies designed primary prevention of chronic conditions is of great to assess the health and nutrition status of adults and focus andconcern [22]. children in the US, are used to monitor the trends in child overweight and obesity [13]. The NHANES EstablishmentofCHL program, however, does not include data from the The Children’s Healthy Living Program for Remote noncontiguous US states of Alaska and Hawaii or the Underserved Minority Populations in the Pacific Region US Affiliated Pacific Island Jurisdictions of American (CHL) is a partnership among the remote Pacific juris- Samoa (AS), Commonwealth of the Northern Marianas dictions of Alaska, AS, CNMI, the Freely Associated Islands (CNMI), Guam, the Federated States of Micro- States of Micronesia (FAS including RMI, Republic of nesia (FSM), the Republic of Palau, and the Republic of Palau, FSM), Guam, and Hawaii to study child obesity the Marshall Islands (RMI) [14]. According to the few among Pacific children, ages 2-8 years. The program is data sources available for the Pacific, the prevalence of sponsored by the United States Department of Agricul- child overweight and obesity combined (≥85th percentile ture (USDA), Agriculture and Food Research Initiative. BMI-for-age) has been estimated at 22% (of 2 – 5 year To address the child obesity epidemic in the Pacific, the olds) in Alaska [15], 32.6% (of 5 – 8 year olds) in Hawaii CHL partners have identified the following program [16], 33.5% (of 2-10 year olds) in the Commonwealth of objectives: 1) Conduct program/data inventories and the Northern Mariana Islands [16], 33.7% (of 2 – 5 year situational analysis; 2) Train 22 professionals and para- olds) in American Samoa [17], and 38.5% (of 5-18 year professionals in obesity prevention; 3) Develop a Pacific Wilkenetal.BMCPublicHealth2013,13:944 Page3of13 http://www.biomedcentral.com/1471-2458/13/944 food, nutrition, and physical activity data management 7) increasedphysical activity. andevaluationsystem;4)Developandconductacommu- 8) lowerprevalence ofacanthosisnigricans (AN). nity-based environmental intervention to prevent, main- tain, or reduce young child overweight and obesity; 5) The CHL intervention targeted the following changes: Evaluate the environmental intervention; and 6) Incur at a reduction in 0.08 of BMI z-score, an addition of 15 leastoneobesitypreventionpolicychangeperjurisdiction. min/day of sleep, a reduction of 0.5 cups/day of SSB, an The focus of this paper is on objectives 4-6, which re- increase of 1 serving/day of fruits and vegetables, an in- late specifically to the rationale and design of a commu- crease of 0.5 cups/day of water, a reduction of 10 min/ nity randomized environmental intervention trial in five day of TV/video viewing, and a reduction of 5% in AN. CHL jurisdictions, and the evaluation of these efforts. The targets are goals of the intervention and provide Intervention planning involves the modification of three guidance for messaging. The differences that the CHL aspects of the environment (social/cultural, physical/ study is powered to detect are provided in the Power built, political/economic) to improve the diet quality and andsamplesize calculations sectionbelow. physical activity level of young children (See Figure 1). Previous randomized controlled trial studies in young The methodology and results of program/data inventor- children, 2-8 years of age, that focused on at least one of ies and situation analysis, critical to the design of the CHL’s primary outcomes, showed a positive effect of strategy and content of the community intervention, has intervention on body mass index (BMI), food intake, been published elsewhere [23]. and/or physical activity (PA) [24-29]. Multiple interven- The investigators hypothesized that children in tionstrategieswereusedinanothercommunitytrialthat communities receiving the CHL obesity prevention were shown to be safe and effective in reducing un- intervention would differ from their counterparts in healthy weight gain in children, without increasing communities not receiving the CHL obesity prevention health inequalities [30]. That study included efforts to intervention. All successful components of the CHL modify children’s food intake and physical activity, and intervention are planned to be implemented in the parental involvement with the children around food and comparison communities after the trial is completed physical activity. However, data on PA expenditure and (i.e., delayed “optimized” intervention). Specifically, the on overall diet quality of participants in these trials are investigators hypothesized that, relative to children in limited. In addition, the populations included in most of the comparison communities, children in the interven- these studies are whites in the US, Australia, or Europe. tion groupwillhavethefollowing differences: There is little known on the efficacy of such actions in remote diverse populations of Pacific Islander, Native 1) lowerweight andBMI velocities. Hawaiian or Alaska Native ethnicity. CHL will be able to 2) increasedsleep. fillthesegapsinthepeerreviewed literature. 3) reduced consumption ofsugar-sweetened beverages(SSB). Methods/Design 4) higher fruitand vegetableintake. The CHL Community Randomized Trial is an environ- 5) higher water intake. mental interventiontrial infive jurisdictions: Alaska,AS, 6) reduced TV/videoviewing. CNMI, Guam, and Hawaii. The Freely Associated States Environmental Promote Outcome Changes Social/Cultural Environment Prevent Possible examples: Healthy Early (cid:129) Family, teachers, leaders, Food Intake chiefs, elders & other Childhood respected role models setting example of healthy living Obesity Political/Economic Physical Environment Activity Possible examples: (cid:129) Change government policies to promote healthy lifestyle Physical/Built Environment Possible examples: (cid:129) Ensure water fountains are available and maintained Figure1TheChildren’sHealthyLivingProgrammodeltoinfluencemultipleaspectsoftheenvironmenttopromotehealthyfood intakeandphysicalActivityinyoungchildren(2-8years)asamethodtopreventearlychildhoodobesityintheUSAffiliatedPacific. Wilkenetal.BMCPublicHealth2013,13:944 Page4of13 http://www.biomedcentral.com/1471-2458/13/944 of Micronesia, which includes FSM, the Republic of evidence that children live and go to school in the same Palau, and RMI, will conduct elements of the CHL sam- community (i.e., not a commuter community), ensuring pling framework and measurements to provide preva- that the measured children have an opportunity to be lence data, but are not engaged in the community exposed to the intervention; aminimalrisk of contamin- intervention trial. The CHL Program was designed to ation between matched-pair communities; having rea- monitor and evaluate the prevalence of obesity in the sonable accessibility for the CHL team (e.g., isolated region through the baseline and follow-up data, while communities that would require substantial travel logis- testing the intervention for impact by comparing inter- tics were excluded); community cohesiveness [36]; hav- ventionwith non-intervention communities. ing sufficient settings for intervention (e.g., community The community intervention activities are quantita- centers, parks, churches, and stores); and for the FAS, tively and qualitatively evaluated [31] in Alaska, AS, scheduled air or boat service. A list of all eligible com- CNMI, Guam, and Hawaii to determine the impact munities was created in each of the jurisdictions based of the intervention. The intervention was developed ontheabove criteria. through blending findings from a community engage- Communities in each of the five jurisdictions were ment process that allowed the community to identify selected to participate in the intervention trial. In and prioritize strategies [23] and review of evidence American Samoa, CNMI, Guam and Hawaii, four basedliterature. communitieswere selected, whiletwo communitieswere Institutional Review Board approvals from the Univer- selected in Alaska due to large distances between sity of Alaska Fairbanks, University of Guam, and Uni- sites. The communities were matched to form pairs versity of Hawai‘i at Manoa were attained prior to data (1 matched-pair in Alaska and 2 matched-pairs for the collection. The American Samoa Community College other jurisdictions; see Figure 2). The pairs were formed andtheNorthernMarianasCollege,andtheinstitutional by matching communities on the following factors: per- partners in the Freely Associated States of Micronesia centage in poverty based on U.S. census, population ceded their Institutional Review to the University of density based on U.S. census, distance from urban cen- Hawai‘iatManoa. ters, and percentage overweight/obesity, when available. In addition, approvals for working with teachers and In each pair, one community was randomly assigned to parentsofHeadStart(aUSfederallyfundedprogramthat intervention and the other to a delayed optimized inter- educates preschool-age children and their families) and vention (community will receive intervention at the end government-sponsored Early Childhood Education pro- ofthemaintrial). grams in the Freely Associated States of Micronesia were Randomization to intervention, in general, produces received in coordination with the program directors and/ study groups that are comparable with respect to orboards,whenappropriate.Otherlocallevelagreements confounding variables [37]. An independent statistician included approvals from the chiefs (matai) and ministers performedtherandomization. (faifeau) of participating American Samoan villages and Two additional non-matched communities (third and themayorsinparticipatingvillagesinGuam. fourth for Alaska and fifth and sixth for other jurisdic- tions) were selected from the eligible list to serve Siteselectionprocess as temporal indicators of anthropometry status (see Communities were identified in Alaska, American Figure 2). Generally, the communities selected for tem- Samoa, CNMI, Guam and Hawaii using the 2000 US poral assessment had been considered to participate as a Census tract data since 2010 data was not available at matchedpair;however,theyoftendidnotmatchanother the census tract level [32] at the time that sites were se- eligible community well or they had less community co- lected in 2011. In the FAS, 2010 country census data hesiveness, which wasnot as important for a community were usedto informselection of sites for prevalencesur- providing prevalence information only. The temporal vey data collection [33-35]. Community selection was communitieswillnot receive theinterventionprogram, based on the following eligibility criteria: population size In the FAS region, 3-5 communities were selected for of >1000, >25% of the population of indigenous/native collection of baseline (prevalence) survey data in each of descent (15% in Alaska due to no census tract with a Chuuk, Kosrae, Pohnpei, Yap, Palau and the RMI population of more than 1000 having more than 25% in- (n=200children per location), accordingto the same cri- digenous/native), and >10% of the population under age teria, plus a criteria of geographic representation. A total 10 years (based on combining census tract data groups of 27 communities will provide baseline (prevalence) of < 5 years of age and 5 – 9 years of age, in order to surveydata from theFAS. have sufficient population size for CHL target of 2 to 8 Thus, in total, four communities in Alaska and six year olds). Additional selection criteria included having communities in each of the remaining four CHL inter- adequate settings for sampling children (e.g., schools); vention jurisdictions were selected for a total of twenty- Wilkenetal.BMCPublicHealth2013,13:944 Page5of13 http://www.biomedcentral.com/1471-2458/13/944 Jurisdiction Community Selection Temporal Communities (n = 6)* (n = 2) Planning Matched Pair Communities (n = 4) Intervention Communities Delayed OptimizedIntervention (n = 2)† Communities (n = 2)† Baseline Participant Recruitment, Baseline Abbreviated Baseline ention InterventionAnd CoMmemausunriteym Aesnstesssment Measurements ated States of valence Survey Interv (n = 2)† Follow-up Measurements Abbreviated Follow-Up Freely AssociMicronesia Pre Follow- Measurements up Analysis Delayed OptimizedIntervention (n = 2)† Figure2Children’sHealthyLivingProgramstudydesignschematic.*Alaskawillonlyinclude4communities.†Alaskawillonlyinclude1 community. eight communities across the CHL region for participa- an F test of the interaction term of intervention group tion in the CHL community intervention trial: 9 and time from a mixed model of the outcomes, account- matchedpairs(18sites total) and10temporalsites. ing for the clustering in a group-randomized trial (GRT) A cross-sectional sample of children in each of the by adjusting the test degrees of freedom to the number CHL intervention communities is being assessed for of communities [39]. The calculations assume a mini- outcomes at baseline and at 24 months (18 months mum n of 150 children with anthropometry and a mini- post-intervention). Additionally, the outcomes are being mum n of 100 children with accelerometry and food and assessed in the FAS region to provide prevalence activity logs in 6 communities in four jurisdictions and information. in two communities in Alaska; this assumption is con- Theinterventiondoesnot explicitly target theassessed servative as the goal is a sample size of 180 children per children;they serve asrepresentatives oftheircommuni- community. An expected correlation for communities ties. Children who participate at both time points pro- within jurisdictions was low with an estimate of the vide repeated measures and serve as an embedded interclass correlation coefficient (ICC) that varied be- longitudinalsample. tween 0.02 to 0.04. We assumed a critical level of 0.05 (two-sided), a power of 80%, and a constant sample size Powerandsamplesizecalculations at baseline and at 24 months. The respective effect sizes Samplesizeestimateswerebasedontheneedforasuffi- for an ICC of 0.02 and 0.04 are modest at 0.26 and 0.35 cient number of communities and children in each of for outcomes with n=150. Using means and variances the five jurisdictions to ensure adequate statistical power for the outcomes from previous research [24,40,41], the to detect meaningful differences between intervention minimum detectable differences for the two ICC values arms in overweight and related outcomes (listed previ- were 0.09 and 0.12 for BMI z-score, 21 and 28 minutes ously) overall and for select outcomes within jurisdic- of television viewing, and 11 and 15 minutes of sleep. tions. The effect size (Cohen’s d) [38] was calculated The respective effect sizes for an ICC of 0.02 and 0.04 based on an analysis of 2000 simulated data sets with are also modest at 0.31 and 0.42 for outcomes with children clustered within community clustered within n=100. Using means and variances for the outcomes jurisdiction. The intervention effect was tested based on from previous research [24,40,42,43], the minimum Wilkenetal.BMCPublicHealth2013,13:944 Page6of13 http://www.biomedcentral.com/1471-2458/13/944 detectable differences for the two ICC values were 0.50 and 30% of the sample was targeted from kindergartens and 0.67 servings of vegetables, 0.45 and 0.61 servings of (orpre-schoolswitha sufficientnumber of5yearolds). fruits, 0.45 and 0.60 servings of water, 0.34 and 0.46 servings of SSB, and 33 and 45 minutes of PA with metabolic equivalent values (METs) > 3, based on Studydesign accelerometry. The CHL Program is as an 18-month community randomized environmental intervention trial focused on Participantrecruitmentgoals preventing early childhood obesity and promoting a In order to meet sampling goals for children between healthy diet and physical activity in young children the ages of 2 – 8 years, recruitment activities involve in the Pacific Region (Novotny R PI, USDA Grant schools and other community venues and activities. Re- award 2011-68001-30335, 4/1/2011 – 3/31/2016). The cruitment sites consist of Head Starts, pre-schools/day trial is registered with NIH (Novotny, clinical trial # cares, kindergartens, WIC sites, community health cen- NCT01881373).BaselinemeasurementsbeganinOctober ters and other appropriate venues (e.g., parks and com- 2012.Themeasurementsfocusonbothparticipant(child) munity recreation centers). Recruitment efforts, led by measures and community assessments, and are being CHL staff in each jurisdiction, involve close collabor- repeated post-intervention (October 2015; see Figure 3). ation with community liaisons (e.g., teachers, school The intervention began in January 2013 in intervention staff, program directors, matai, mayors) to enhance par- communities when baseline measurements were com- ticipation and retention throughout the measurement plete. Measurements in the FAS region, focusing on protocol. The teams in all jurisdictions tailored the re- establishing prevalence data for the region, are targeted cruitment strategies to work effectively with the stake- forcompletioninSeptember2014. holder organizations while meeting recruitment goals of All matched-pair communities are assessed during a CHL. The total proposed sample size for anthropometry 12-month baseline measurement period and at post- measures for CHL is 4100 children for the cross- intervention using the same protocol and procedures. sectional samples at baseline and at 24 months. For the Community assessments of each matched-pair commu- embedded longitudinal (individual) design, the intent is nity are conducted within the same time frame as the to collect repeated measurements from 40-50% of chil- child measures. In each matched-pair, intervention com- dren with baseline measurements. To ensure an ad- munities were prioritized for measurement so that the equate representation of 3-5 year olds at baseline for the intervention study phase could commence in January embedded longitudinal sample, 70% of the sample was 2013. Participant and community assessment measure- targeted from Head Starts, pre-schools or day cares mentsarelistedinTable1. Baseline Post-Intervention 0 MONTHS 24MONTHS Individual LevelMeasurements* Individual LevelMeasurements* n=150 intervention 1 n=150 intervention 1 n=150 intervention 2 n=150 intervention 2 n=150 comparison 1 n=150 comparison 1 n=150 comparison 2 n=150 comparison 2 n=150 temporal 1 n=150 temporal 1 n=150 temporal 2 n=150 temporal 2 Community Level Measurements Community Level Measurements Intervention and Delayed Optimized Intervention Intervention and Delayed Optimized Intervention Communities Communities Food inventory and survey Food inventory and survey (without food cost survey) Physical activity inventory and survey Physical activity inventory and survey Community Readiness Assessment Community Readiness Assessment Temporal Communities Temporal Communities None None Figure3TheChildren’sHealthyLiving(CHL)Programindividualandcommunitylevelmeasurementtimeline.*Longitudinalsamplewill beembeddedinthecross-sectionalsample. Table1TheChildren’sHealthyLiving(CHL)Programindividualandcommunitylevelmeasures hW Individuallevelmeasures Assessecdominmmuantitciheesd-pair Assecsosemdminunteitmiepsoral AinsseFsAsSe†d ttp://wwilkenet Category Measurement Measurementtools Completedby 0month 24month 0month 24month w.b al. Demographic Demographic Questionnaire Surrogate* X X X X X iom BMC [15,43-48] ed P Anthropometry WHeeiigghhtt PStoardtaiobmleeStcearle SSttaaffff XX XX XX XX XX central.c ublicHea Waistcircumference CircumferenceTape Staff X X X X X om lth Diet 2[61d,#62F]oodintake Food&ActivityLog Surrogate* X X X /1471-22013,1 43 PhysicalActivity(PA) 6dPA[66] Accelerometer** Child X X X 58/1:944 2d#ActivityLog[62] Food&ActivityLog Surrogate* X X X 3/9 4 Sedentarybehavior(SB)/ScreenTime 6dSB/ST[66] Accelerometer** Child X X X 4 (ST) 2d#ActivityLog[62] Food&ActivityLog Surrogate* X X X UsualSB/ST[52] Questionnaire Surrogate* X X X Sleep 6dSleeping[66] Accelerometer** Child X X X 2d#ActivityLog[62] Food&ActivityLog Surrogate* X X X Sleepingbehavior[53] Questionnaire Surrogate* X X X AcanthosisNigricans Presence/Severity[67] Visualobservation/assessment Staff X X X form Culture Language/culture Questionnaire Surrogate* X X X [49-51] Communitylevelmeasures Assessedinmatched-pair Assessedintemporal Assessedin communities communities FAS† Category Measurement Completedby 0month 24month 0month 24month Food[69-71] FoodOutletInventory Staff X X X FastFoodRestaurantInventory Staff X X X FastFoodObservationForm Staff X X X CHLFoodCostSurvey Staff X X FoodAvailability&MarketingSurvey Staff X X X StoreEnvironmentWalkabilitySurvey Staff X X X PhysicalActivity[69,74] PhysicalActivityFacilityInventory Staff X X X PhysicalActivityFacilityObservationForm Staff X X X P a g e 7 o f 1 3 Table1TheChildren’sHealthyLiving(CHL)Programindividualandcommunitylevelmeasures(Continued) hW ttpilk ParkInventory Staff X X X ://wen ParkObservationForm Staff X X X ww eta .b l. SchoolInventory Staff X X X io BM m C SchoolObservationForm Staff X X X ed P IPnhvyesnictaolryAcfotirviCtyhurchandCommunityCentersUsedfor Staff X X X centra ublicH l.c ea ChurchObservationForm Staff X X X om lth CCoommmmuunniittyyMReeaddiicnaelsFsa[7c8il]ities[76,77] MCoemdimcaulnFiatycilRiteyaIdnivneensstoAryssFeossrmment SKteayffcommunity XX XX X /1471-22013,1 †FAS=FreelyAssociatesStatesofMicronesia. Stakeholders 458/133:944 X=indicatesmeasurementcompleted. /9 4 *Surrogatereporter=parent/caregiver. 4 **Aminimumof100childrenineachmatched-paircommunityandFASjurisdictionwillwearanaccelerometer. #Randomlyassignednon-consecutivedays. P a g e 8 o f 1 3 Wilkenetal.BMCPublicHealth2013,13:944 Page9of13 http://www.biomedcentral.com/1471-2458/13/944 Measurements are collected in either a school setting Participantandfamily/householdcharacteristicsand (e.g., Head Start), or in a community-based setting behaviors (e.g., CommunityRecreationCenter)andrequireamini- At the first visit, in matched-pair and FAS communities, mum of two visits. At the first visit, study participants’ parents/caregivers complete four questionnaires. The parents/caregivers are oriented to the study, provide in- first questionnaire assesses the demographic profile of formed consent and complete questionnaires. Partici- the child including age, race/ethnicity, sex, household pants receive instructions on completing a food and composition, educational level and income of the par- activity log, and on the use of an accelerometer (Actical, ent/caregiver, household food security, religion, general Murrysville, PA). If children are present (e.g., at a health status, and early life feeding behaviors. Questions community-based setting), accelerometers are placed, have been adapted from those previously used in other and anthropometric measures and acanthosis nigricans studies [16,44-49]. The second questionnaire relates to screening are performed, after receiving assent from the the cultural identity of the parent/caregiver. This ques- child. At the second visit, 6 days later, the accelerome- tionnaire was developed for Native Hawaiians and has ters are removed and the food and activity logs are col- been adapted [50-52] to be generalizable to the entire lected and reviewed with the parent/caregiver. Any CHL region. The third and fourth questionnaires on children not measured in visit one for anthropometry usual screen time/sedentary behavior and sleep, respect- and acanthosis nigricans are measured at the follow-up ively, have been adapted from previous studies [53,54], visit. Compensation for study participation was provided with terminology added to the usual screen time/seden- at visits 1 and 2 ($10 each in Hawaii, American Samoa tary behavior [53] and sleep [54] questionnaires for clar- and CNMI and increased by investigators in Guam to ity. The forms are administered in English in Alaska, $20 and in Alaska to $25 based on their determination CNMI, Guam, and Hawaii. In other jurisdictions, the of a locally acceptable level). A similar procedure is forms are translated into other languages. The translated followed in the FAS prevalence study, where $10 is versions of the forms were back-translated as the stand- providedateach of visits1and2. ard protocol [55] to ensure the correct content has been Abbreviated measures are completed in temporal com- conveyed in the translation. In American Samoa, the munities during transition periods between matched-pair formsaretranslatedintoSamoan,andintheFASregion, communities or after all matched-pair community assess- into Chuukese, Kosraen, Marshallese, Onouan, Palauan, ments are completed. The scheduled visits are limited to Pohnpein,UlithianandYapese. one visit, which consists of an orientation to the study, informed consent, the completion of a demographic questionnaire, and the collection of the child’s anthropo- Anthropometryandbodycomposition metric measurements. Measurement settings included Weight, height, and waist circumference are measured bothschoolsettingsandcommunity-basedsettings.Com- by trained research staff based on standardized proce- pensationforparticipationwasprovidedattheendofvisit dures and protocols [56-58]. Zerfas criteria are used to 1($7ineachofHawaii,AmericanSamoa,andCNMI,$10 standardize research staff against the height, weight, inGuamand$25inAlaska).Communityassessmentsare and waist measurement of a certified anthropometrist notconductedinthetemporalcommunities.Additionally, (Novotny R, CHL PI) [59]. Zerfas provides no waist cir- recruitment group leaders (teachers, community leaders) cumference criterion; however, the uniform criterion areprovidedwith$20fortheirassistancewithrecruitment assigned to all assessments measured in cm (mm) units groupsinalljurisdictions(includingtheFAS). is used. No research staff can assess children for a meas- urefor which theydidnot passthe Zerfascriteria. Individualleveloutcomes Participants wear lightweight clothing and no shoes, Anthropometric changes are the primary health out- and empty their pockets. Height is measured to the comes of the study, and anthropometry is measured in nearest 0.1 cm using portable stadiometers (Perspective all communities. Diet, physical activity, and sedentary Enterprises, PE-AIM-101; Portage MI). Weight is mea- behavior are additional primary behavioral outcomes sured to the nearest 0.1 kg using portable scales (Seca measured in matched-pair and FAS communities. Sleep Model 876; Chino CA). Plastic tape (Seca Model 201; and acanthosis nigricans are secondary outcomes mea- Chino CA) is used to measure waist circumference at sured in the matched-pair and FAS communities. All the level of the umbilicus to the nearest 0.1 cm [56]. field research staff underwent measurement training and Weight, height, and waist circumference measurements standardization of anthropometric measurements, and a are measured three times; three additional measures are thorough review and testing of protocols and procedures made if there are no two measures among the original were conducted, before baseline measurement collection three within 2 units (e.g., 0.2 kg for weight). These wasinitiated. measures are used to compute Body Mass Index (BMI) Wilkenetal.BMCPublicHealth2013,13:944 Page10of13 http://www.biomedcentral.com/1471-2458/13/944 as weight (kg) / height (m)2, waist (cm) to height (cm) situations where the device comes off, is removed or has ratios, and subsequently BMI z-score, waist circumfer- to be replaced. At the conclusion of data collection, the ence z-score, BMI-for-age-percentiles, and waist circum- accelerometer data are processed using the manufac- ference-for-age percentiles [60,61]. turer’s software (Actical version 3.0) with output activity incounts/minute. Research staff instruct parents/caregivers to record Dietaryintakeofchildren their child’s activities for the same two days in which Food logs (i.e., dietary records), reported by a surrogate food intake is recorded on the FAL. Parents are (parent or other caregiver), are used to assess energy, instructed to provide the start and end time and details nutrient, and food group intake of the child. The format of each activity, including sleep and screen time, and methods used for the food logs have been adapted throughout a 24-hour period. Activity data are entered from previous studies [62,63]. The food log is combined using PacTrac3, which calculates minutes of activity by with an activity log in an easy-to-carry booklet, referred intensitylevelandMETs. to as the Food and Activity Log (FAL). Parents/care- givers are asked to complete the FAL for their children on two randomly assigned non-consecutive days, which Acanthosisnigricans(AN) include weekdays and weekend days, between visit 1 Participants’ necks are examined for the presence of AN and 2. Assignment of recording days is based on the day by two trained research staff. Using Burke’s quantitative of the child’s first visit (Monday – Saturday). Standard scale for AN, a score is given for AN severity: 0 to 4 techniques are used to improve accuracy of information [68]. Participants with a score of one or higher are con- recorded in the FAL [64]. Parents/caregivers are sidered tohaveAN.ANisindependentlyassociatedwith instructed in record keeping techniques with the aid of hyperinsulinemia, an important risk factor for type 2 food models, service ware, and utensils. Parents are pro- diabetes [69], so parents/caregivers of participants with a vided a tool kit of calibrated utensils (i.e., measuring positive screen for AN are provided with a referral to cups and spoons); the FAL; and a Ziploc® (Racine WI) follow-up with their children’s health care providers or a bag in which to place food wrappers, labels, and pack- public healthserviceprovider. ages (WLP). CHL staff follow-up with reminder tele- phone calls. During visit two, research staff review the Communityleveloutcomes FAL with the parents (e.g., for completeness of food en- Communityassessmenttoolkit(CAT) tries, portion size estimation, food preparation methods, The CHL CAT has been created to evaluate the food accuracyofrecordingdata). Staff are trainedto enter the and physical activity environment of each matched-pair FAL data into the Pacific Tracker3 (PacTrac3) dietary and FAS community. The evaluation of the food envir- and physical activity assessment program [63]. Data onment includes an inventory and survey of fast food from the PacTrac3are used to calculatefood groups and restaurants and food outlets adapted from surveys from nutrients using a food composition database developed the CX3 and BTG (Bridging the Gap) programs (see by the University of Hawaii Cancer Center for use in the Table 1) [70-73]. A food cost survey, adapted from the Pacific region[63,65,66]. Alaska Food Cost Survey [74], is also being conducted. The evaluation of the physical activity environment Childactivity includes an inventory and survey of physical activity The Actical accelerometer (Z series, Phillips Respironics facilities, parks, schools, and churches and community Inc; Murrysville PA) is a small, lightweight, water resist- centers used for physical activity, also adapted from ant,omni-directional device capable ofmeasuring move- surveys from the BTG program (see Table 1) [70,75]. A ment in multiple planes and providing data on intensity, walkability checklist has been adapted from a U.S. frequency, and duration of activities in young children Department of Transportation Federal Highway Admin- [67]. Devices are initialized to save data in 1-second istration and National Highway Traffic Survey Adminis- intervals to record spontaneous movements of young tration survey [76]. An inventory of medical facilities in children. The device is worn on the participant’s the region is also included, adapted from a survey from non-dominant wrist attached with an Ident-A-Band the CHANGE (CDC Community Health Assessment (tear-resistant; Hollister; San Fernando CA) plastic band. and Group Evaluation) program [77]. Staff conduct ini- Participants are asked to wear the device daily (without tial information gathering for inventories using on-line removal) until it is removed by research staff 6 days resources followed by in-person visits to complete the later. The participants and their parents/caregivers are inventories and to perform the surveys. The information assured that the devices could be worn while bathing, from the CAT is used to inform the design of the inter- swimming or sleeping. Extra bands are provided for vention and is used to aid in the interpretation of results
Description: