Anaesthesia doc - aagbi PDF
Preview Anaesthesia doc - aagbi
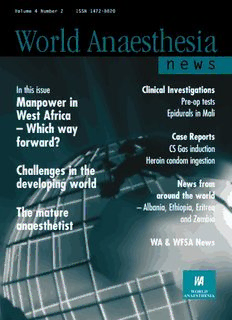
Volume 4 Number 2 ISSN 1472-8820 World Anaesthesia n e w s In this issue Clinical Investigations Manpower in Pre-op tests West Africa Epidurals in Mali – Which way Case Reports forward? CS Gas induction Heroin condom ingestion Challenges in the developing world News from around the world – Albania, Ethiopia, Eritrea The mature and Zambia anaesthetist WA & WFSA News W elcome to World Anaesthesia News “Anaesthesia Worldwide” has now metamorphosed into “World Anaesthesia News” with Contents a new look and a new international editorial board. It is no longer the journal of the World Federation of Societies of Anaesthesiologists (WFSA) but is supported by a generous grant from the Federation. Feature articles Anaesthetic manpower in West Anaesthesiologists are often confused by the relationship between the WFSA. and World Africa 1 Anaesthesia. I hope that the articles in this issue on each of these organisations will make matters clear. Essentially, the WFSA is a federation of societies of anaesthesiologists as its name Challenges in the developing world 2 suggests whilst World Anaesthesia is a group of individuals with similar aims, namely “to make available the highest standards of anaesthesia to all the peoples of the world.” Naturally, the two The mature anaesthetist 4 organisations work closely together and try to support each other’s endeavours. This issue of World Anaesthesia News continues the tradition of publishing articles from News from around the world individuals and societies in developing countries. At the end of these articles (from Ethiopia, A message from Albania 6 Eritrea and Zambia) I have added a few statistics on gross domestic product (GDP), infant A history of anaesthesia services mortality and life expectancy. The figures are all too familiar: GDP is under US $1000 per in Eritrea 7 capita, infant mortality approaches 100/1,000 and life expectancy is less than 50 years. In the developed western world, comparable figures are GDP $20-30,000, infant mortality 5-6/1,000 A letter from Ethiopia 8 and life expectancy 70-80 years. The figures for parts of Eastern Europe and the former USSR The WFSA in Zambia 9 lie somewhere in between. With so little available to be spent on health, it is easy to be pessimistic but all the authors remain optimistic about the future in their countries Clinical investigations I would also commend to you Prof. Thara Tritrakarn’s essay, based on a talk he delivered Epidural anaesthetic practice at the World Congress in Montreal in June. He concludes that if we in the West can help train in Mali 11 a single anaesthetist who returns to his or her home country, we will have made an immeasurable contribution to the improvement in health care in that country. There is our Pre-anaesthetic tests in ASA I and ASA II patients 12 challenge for the new millennium. The editorial board and I look forward to hearing your thoughts, critical or otherwise of Case Histories our efforts and of receiving your contributions to future editions of World Anaesthesia News. Anaesthetic consideration of William F Casey Heroin condom ingestion 14 CS Gas induction of anaesthesia 15 Useful information 16 The editor of World Anaesthesia Dr Rob McDougal (Australia) Anaesthetic websites to try 18 News is: Email: Dr W F Casey [email protected] Feature Extra Popes Cottage Gassing in Guinea Cheltenham Rd Dr Tom Ruttmann (S.Africa) – on and off ship 19 Gloucester GL6 6TS, UK Email: [email protected] A detached retina in the land Tel: (+44) 01452 814229 of yaks and yetis 21 Fax: (+44) 01452 812162 Dr Iain Wilson (UK) Pigs might fly! 22 Email: wfcasey@[email protected] Email: [email protected] The WFSA 23 Editorial Board Editor Emeritus The constitution of World Dr Dixon Tembo (Zambia) Dr Roger Eltringham (UK) Anaesthesia 24 Email: [email protected] Email: [email protected] A letter from Dr Iain Wilson 25 Book Review 12 Prof. Rebecca Jacob (India) Submissions to World Anaesthesia Email: [email protected] News may be sent to any of the above. Anaesthetic Manpower in West Africa s e i – which way forward? r o t S e commenced in 1970 and at the West years with only 6 Fellows of Anaesthesia; a r Dr O A Soyannwo & Prof. E O Elegbe u African Medical College in 1979. In their ratio of 1:49. Department of Anaesthesia t early years, both colleges produced a total of The Diploma in Anaesthesia a University College Hospital e 75 fellows in Medicine and Surgery but programme of the West African College of F Ibadan, only one in Anaesthesia. We have looked at Surgeons, a constituent College of the West Nigeria. the impact of the West African Postgraduate African Post-graduate Medical College Email: [email protected] Medical College training on anaesthetic (WAPMC) was commenced in 1990. This manpower development. programme yielded 56 diplomats within the 5 years studied. However, 30 (53%) of these Introduction Methods and Material diplomats were also pursuing the Fellowship Since the introduction of ether in 1846, The number of candidates who registered programme. anaesthesia has witnessed many for the examination of the West African innovations in the drugs, equipment and College of Surgeons Fellowship in Discussion techniques used. The Schimmelbusch mask, Anaesthesia from April 1992 – October Postgraduate medical education based in the EMO and standard Boyles machine have 1995 was collected from the West African West African sub-region has been pursued been replaced with computerised anaesthetic Postgraduate Medical College. The records with vigour since the early 60s by experts in and monitoring equipment for the safe were reviewed to establish the number of all specialties. These teachers, who generally administration of anaesthesia. The wider candidates that actually attempted and those had their training in overseas institutions, range of drugs available allows a flexibility of who passed examinations of the College in were determined to train their junior techniques suitable for novel and April and October of each year. The ratios colleagues locally at reduced cost to provide demanding surgical procedures and patients’ of anaesthetist to surgical graduates were improved medical services. The dearth of varying medical conditions. Thus, advances determined. The number of anaesthetists anaesthetists has, however, continued, with in surgery have been possible largely due to trained through the Diploma programme the ratio of anaesthetists to the general modem anaesthesia. over the same period was also obtained and population being at least 1:300,000 Many of the early pioneers of the number that proceed to the Fellowship compared to 1:10,000 in developed anaesthesia were surgeons like James programme was determined. countries. In a recent survey of 52 hospitals Simpson, physician to Queen Victoria, who in 15 states of Nigeria, nurse anaesthetists popularised the use of chloroform. By virtue Results provide service with physician anaesthetists of their eminent position in the medical The Faculty of Obstetrics and in 50% of hospitals and were the sole world, they advocated and championed the Gynaecology attracted the highest number providers of anaesthesia in 20% of the use of anaesthesia, sometimes against of postgraduate trainees with a steady hospitals including some teaching hospitals. considerable opposition. increase in the number of candidates Although nurse anaesthetists provide useful The Association of Anaesthetists of attempting the examinations from 275 to assistance to physician anaesthetists in many Great Britain and Ireland was founded in 312 candidates over the five years of the parts of the world, strict guidelines are 1932, whilst the first examination for the survey. There were between 91 and 101 necessary to ensure the safety of patients. In Diploma in Anaesthesia was held in 1935, candidates at Part 1, 22 to 58 at Part 2 the Gambia, surveys have shown that the same year that a chair in anaesthesia was and 16 to 40 Fellows produced per year. problems such as post-operative fluid and created in Oxford. The status of anaesthesia This was closely followed by the Faculty of electrolyte imbalance, septicaemic shock, in Great Britain, on a par with other Surgery producing 16 to 39 Fellows per difficult airways and intercurrent medical medical and surgical specialties, was secured year. Anaesthesia had only 9 to 27 diseases occur in 65% of surgical patients in 1948 with the introduction of the candidates at Part 1, 17 to 26 at Part 2 and require the expertise of physician National Health Service. Since then, and zero to 2 Fellows per year. A total of anaesthetists if outcome is to be improved. anaesthesia in the developed countries has 2,963 candidates sat for the primary Anaesthesia as a career is unattractive advanced very rapidly, become very safe and examination of the various surgical to both medical students and interns thus allowing advances in surgery. specialties viz. Obstetrics and Gynaecology, because of the “behind the scene” nature of In West Africa, training of Surgery, Dental Surgery, Ophthalmology the specialty and their lack of adequate anaesthetists locally to Diploma level and Otorhinolaryngology, but only 93 exposure to it during their training. commenced in 1967 with the creation of candidates sat the anaesthetic primary. This Unfortunately, the areas where anaesthetists the first autonomous Department of produces a ratio of 32 prospective surgeons are primary care providers such as in Anaesthesia at the University of Lagos. Post- to l anaesthetist. The end point of the Intensive Care, Resuscitation, and Pain graduate fellowship training in Nigeria training produced 292 Surgical Fellows in 5 Therapy Clinics are poorly developed or 1 non-existent in most African hospitals. they then may find the specialty postgraduate training in surgical specialties, F Thus, the few doctors that join the specialty interesting and fulfiling as a potential only a few are interested in anaesthesia. It e a find the work unrewarding especially when career. was initially thought that one year’s training tu they are presented with poorly prepared The Diploma in Anaesthesia to Diploma level might ease the manpower r patients, have a restricted range of programme should be re-structured and shortage but since the training is based at e anaesthetic agents with little monitoring supported by Governments. For example, tertiary institutions, most of the trainees s equipment and inadequate resuscitation medical officers already in service could be decide to continue to the Fellowship t o faculties. It is, therefore, not surprising that sponsored during their training and then be programme and this reduces the number of r i despite the efforts of many within the sub- made to serve for a specified period in clinical anaesthetists working in the e s region, the specialty remains unattractive. government hospitals before they would be secondary level of health care. Many of the few locally trained anaesthetists eligible for further sponsorship for the quickly migrate from West Africa to more Fellowship programme if that is what they Conclusion attractive areas where there is a shortage of wish. Such a move will not only provide Advances in surgery have been anaesthetists. Even our locally trained improved services at the secondary level of possible largely due to innovations in Diplomats have found favour with the health care delivery but will reduce the drift modem anaesthesia. However, whilst there Nigerian Government’s technical assistance of trained anaesthetists into urban private are enough anaesthetists in most scheme and they are sent to work in other hospitals. developed countries to allow sub- countries. At the tertiary level, accreditation specialisation there is profound shortage of What then is the way forward when criteria for surgical departments should anaesthetists in West Africa. The situation anaesthetists are under pressure to provide require adequate anaesthetic and resuscitative is being made worse as few undergraduates services for sicker patients undergoing an facilities in the hospital. West African or new medical graduates are willing to increasing range of surgical procedures? countries with compulsory National Service consider anaesthesia as a future career. At a Only a combination of strategies can Schemes should allow the year to be spent in recent meeting of the West African redress the widening gap between the anaesthesia and other specialties with chronic College of Surgeons in Conakry, Guinea numbers of trained anaesthetists and manpower shortages. Further, efforts must in 1999, 146 new fellows were admitted surgeons in the sub-region. Since medical be made to ensure that essential facilities for to the College, six of whom were education should respond to the health the safe practice of anaesthesia be provided at anaesthetists, a ratio of 1:24. Of the six, needs of the community, the time all levels of health care and that those who three were Nigerians, 2 were from Guinea allocated solely to anaesthesia in the provide it are financially adequately and 1 from Gabon. medical students curriculum should not be remunerated. These measures will not only less than eight weeks and the specialty promote the growth of anaesthesia in the Acknowledgement should form one of the options for intern sub-region but also improve standards in We wish to thank Professor Kayode Odusote. training before full registration. New surgery and critical care medicine. Secretary, West African Postgraduate Medical graduates should have an opportunity for This study has further confirmed that College for his invaluable assistance in data locum appointments in anaesthesia and despite the large number of doctors seeking collection. Challenges in the Developing World Prof. Thara Tritrakarn little access to anaesthetic services. Many capita in US dollars in 1999. Countries with a lives are lost because surgery and high GNP have plenty of doctors, low patient Siriraj Hospital, anaesthesia are inaccessible to patients and per doctor ratios and low infant mortality Mahidol University, their families. There is a great shortage of rates. In countries with lower GNPs, the Bangkok, anaesthetists in every developing country number of patients per doctor and the infant Thailand with ratios as high as 1 million potential mortality rises. Email:[email protected] patients to each anaesthesiologist. Without In countries with a low per capita GNP It is 154 years since the birth of anaesthesia adequate anaesthesia, surgery cannot (below US $1,000 per annum), priority is on October 16th 1846 when ether was first progress and the health and welfare of usually given to primary health care to reduce used. Anaesthesia has contributed to the millions of people suffers. the incidence of infectious diseases, to advances made by all branches of surgery, reduce maternal and infant mortality and to intensive care and pain management and, in Economics and Anaesthesia reduce malnutrition. Anaesthesiology is the developed world, anaesthesiologists are Economic, political and social factors ignored. In Laos, ten anaesthesiologists serve respected and highly paid members of the influence the priority given to health care and a population of 5.3 million, in Cambodia, 20 medical profession its various specialties including anaesthesia. anaesthesiologists seek to serve 10 million On the other hand, in many parts of the In Table 1, thirteen countries are listed by the and in Bhutan, there are no physician developing world, would-be patients have gross national product (GNP) or earnings per anaesthetists at all. What few anaesthetists 2 Table 1: Relationship of economy to health care indices and anaesthesia manpower s Country GNP/US$ Pop. Infant mortality Pt. per doctor No. anaesthetists Pt. per anaesthetist Nurse anaesthetists e i USA 31,400 273m 7 387 23,300 11,500 Yes r o Japan 30,300 126m 5 522 4,200 20,000 No t s Singapore 21,800 4m 5 667 130 26,000 No e Hong Kong 24,700 6m 5 772 150 40,000 No r u Malaysia 3,100 22m 12 1,477 250 88,000 No t a Thailand 1,850 62m 26 2,461 500 124,000 Yes e F Indonesia 460 207m 60 6,786 350 591,000 Yes Pakistan 492 136m 88 2,000 400 340,000 No Laos 258 5m 94 4,300 10 500,000 No Bangladesh 289 130m 90 12,500 200 650,000 No Vietnam 310 79m 34 2,300 400 197,000 Yes Cambodia 270 10m 110 9,000 20 500,000 Yes Nepal 225 23m 88 12,000 80 287,0000 No Drugs and equipment there are, work in teaching hospitals in large equipment and serve the poorer sections of cities. In smaller towns and cities, surgeons the community. In smaller cities, anaesthesia Selecting appropriate drugs and equipment is or general practitioners, nurses or technicians is often administered by nurses or another challenge for anaesthesiologist who administer anaesthesia. Surgical mortality is technicians working under the supervision of have trained in western or developed high and the risks of anaesthesia often medical doctors or entirely unsupervised. In countries and grown used to using state-of- exceed those of surgery. countries such as Thailand, Indonesia and the-art drugs and equipment. With limited In countries with a moderate per capita China, nurses administer 70-90% of budgets, cost benefit ratios have to be GNP (US $1,000-10,000), more money is anaesthetics. carefully considered. Propofol and available to be spent on health and Anaesthesiologists in developing sevoflurane cost 20-30 times more than secondary and tertiary care receive some countries work very hard. They strive to thiopentone and halothane. Is a slightly priority. Hospitals are better equipped and offer safe anaesthesia to their patients shorter awakening time worth that extra staffed and specialisation is encouraged. despite having a limited range of drugs and cost? Anaesthetists are in high demand but few in equipment. They are, in addition, often Electronic monitors frequently break number and rarely work outside large cities. responsible for patient care in Intensive down if not properly maintained and they are Only in countries with a high GNP are there Care Units, for supervising nurse costly to repair. Anaesthesiologists in sufficient anaesthetists but their services can anaesthetists, purchasing drugs and developing countries must decide what are be very expensive. equipment and being responsible for the the most appropriate monitors for them. maintenance and repair of equipment. Pulse oximeters detect hypoxia before clinical Anaesthesia in the developing Journals and textbooks are scarce and signs are evident and are probably of greater world opportunities for post-graduate education, value as the sole monitor than an ECG, The ultimate goal of anaesthesiologists is the either at home or abroad, are few and far capnograph or oxygen analyser. same worldwide: “the provision of safe between. Research is difficult or anaesthesia for all.” It is much easier to impossible. Their status and income is Human resource development. achieve this goal in rich and developed often lower then that of surgeons and Many developing countries do not know how countries where anaesthesiologists are not physicians and many anaesthesiologists many anaesthetists they need but should only equipped with knowledge but have the have to undertake several jobs to earn implement a realistic human resource plan drugs, equipment and support facilities they enough to support their families. for anaesthesia. The mix of the workforce need. Like other health professionals they should be made explicit: whether all enjoy good working conditions and have Politics and health care. medically qualified anaesthetists or is there a sufficient income to maintain their families In the developing world, when governments continuing need for nurse anaesthetists. In and their social status. change everything including health budgets countries where there is a shortage of In less affluent, developing countries it and priorities change. It is essential for doctors, an entirely medically qualified is a greater challenge. Anaesthetic practice anaesthetists to win the support of anaesthetic work force is inappropriate and can vary considerably, even within a given politicians and the community at large and to nurse anaesthetists are vital and county. In the larger centres, medical schools, impress on them the importance of indispensable. Appropriate and concurrent teaching hospitals and private clinics are anaesthesia to public health if they are to plans for their development have to take usually well equipped. Public hospitals often make any substantial improvements in place alongside those for physician have poorer facilities, fewer drugs and less patient care. anaesthetists. 3 Because of low income, low Australia in the Pacific and France in The Mature F professional status and a perceived lower francophone Africa. e a quality of life, anaesthesia remains an To prevent and influx of foreign medical t unattractive profession. Support for its graduates to the United States, increasingly Anaesthetist u r development from politicians, government difficult and expensive examination hurdles e and health providers is essential. Foreign have been introduced (ECFMG & USMLE). s support may also be initially needed to start Only the most determined foreign medical t o and develop suitable training programmes. graduates are able to enter the United States Rebecca Jacob r i and they often find themselves involved in Professor & Head, Dept of Anaesthesia es Improve professional esteem sophisticated basic research divorced from The Christian Medical College and Hospital and popularity clinical medicine and irrelevant to the actual Vellore, Anaesthesiologists in the developing world practice of medicine in their home countries. India must constantly prove to their surgical The gap between clinical medicine in the Email: [email protected] colleagues their ability, knowledge, skill and United States and in developing countries is professionalism. Their contributions to becoming wider by the day. Among the definitions of the word Intensive Care, trauma management, In the United Kingdom, the fees “mature” given in Chambers Dictionary resuscitation and pain management will charged to foreign students were are “full development” or “perfection”. gain them recognition and win them dramatically increased in the 1990s to Maturity and chronological age do not professional esteem. They must show £17,000 (US $25,000) per year and continue necessarily go together. We associate youth medical students and young doctors that to increase by 10% per year. These with quick motor function but a certain anaesthesia is an interesting and exorbitant fees are an effective barrier amount of ineptitude. Conversely, we intellectually satisfying branch of medicine preventing students travelling to the UK to associate age with experience and common combining anatomy, physiology and study medicine and anaesthesia. The image sense and hope that, as we mature, pharmacology with a clinical knowledge of of the generous British gentleman experience and common sense added to our medicine and surgery and technical encouraging learning and scholarship will basic knowledge will more than compensate anaesthetic skills. Anaesthesia makes gradually change that of the stingy, niggardly for our slowing motor function. surgery possible and safe, relives patients and selfish profiteer. If changes do not occur Anticipation and the prevention of problems of pain and saves lives from trauma and in the USA and the UK, immeasurable become the norm. critical illness. damage will be done to medical education in Sometimes though, experience doesn’t the developing world. go hand in hand with common sense. We External help may take unnecessary risks such as not In 1950, the World Health Organisation Give a helping hand wearing gloves when obtaining intravenous (WHO) established an anaesthesia training More than half the world’s population has access. How many of us ‘mature’ centre in Copenhagen, Denmark. It ran a one very limited access to anaesthetic services anaesthetists have encouraged our junior year training course for anaesthetists from but there are a large number of anaesthetists colleagues to get immunised against hepatitis developing countries until 1973. Many in the developed world who can help their and have not got immunised ourselves? doctors completed the course and then colleagues assist these people. Universities, So, what are the qualities associated returned home to become the pioneers of national societies and organisations and with maturity? I would suggest they include anaesthesia in their homelands. Some, individuals can play an active role in the a lot of common sense coupled with however, gained specialist qualifications development of anaesthesia not only at professional skills, confidence, and an ability and decided to stay in the West and enjoy a home but also at a regional and world to maintain good interpersonal relationships more affluent life-style than would be community level. If only 1% of them helped and to work as part of a team. Coping with possible at home. train a single anaesthetist from a a stress is also a major element of maturity. More recently, the World Federation of developing country who then returned home Managing a family and having a Societies of Anaesthesiologists (WFSA) has to train their juniors, the standard of fulltime job can be extremely stressful. When been active in establishing training courses anaesthesia in their respective countries we are young, we make the decision to find for anaesthetic personnel around the world. would rise immeasurably. But be careful; do a partner, have children, and perhaps drop The Bangkok Anaesthesia Training Center not give them internationally recognised and out of “the system “ for a while. When we (BARTC) was established in 1995 by the marketable qualifications. It is human nature resume our professional careers there is WFSA and the Royal College of to seek to emigrate to where one can enjoy inevitably conflict between our professional Anaesthesiologists of Thailand (RCAT) to a higher standard of living. Encourage them and family responsibilities. In my country, train anaesthesiologists from similar to go home and help their fellow very rarely does a woman give up her countries (Laos, Cambodia, Vietnam) who countrymen. profession because of domestic pressures. would then return home and become the The joint or extended family usually helps future trainers in anaesthesiology, thus This essay is based on a talk given at the out and the ready availability of dependable raising standards in their respective World Congress of Anaesthesiolgoy, Montral live-in maids is also a great help. Yet the countries. Other developed countries have 2000. The bold print above is mine, not the worries of having a sick child at home, helped elsewhere: Canada in Nepal, author’s (Ed) attending parent/teacher meetings, preparing 4 Electronic for school examinations or handling woman as they are to a man. Irrespective of s recalcitrant teenagers are all part of the whether the primary cause of stress is dom- e process of maturing and learning to cope. estic or professional the two often interact ri The older anaesthetist may often has causing profound consequences to both. Publication of o t to cope with intercurrent illness such as It has been said that it is very lonely at s diabetes, ischaemic heart disease or arthritis the top: it is, but it is very challenging as e and remember to take a handful of tablets well. Find ways of dealing with the “Update in ur every night Living with busy on-call associated stress. Find a partner, friend or t a schedules and the inevitable disruption of colleague to whom you can unload your e sleep also becomes increasingly difficult. troubles and frustrations without fear of it Anaesthesia” F What about the “normal’ business of being misconstrued or repeated elsewhere. menopause? Only those who have gone Develop skills of control, assertiveness and through a stormy peri-menopausal period diplomacy. It is important to learn to can understand the feeling of inadequacy, respond appropriately to verbal aggression. l “Update in Anaesthesia” is an education the inability to react rapidly in a situation Non-verbal behaviour and body language are journal produced by “World Anaesthesia”, which was formerly considered a challenge important in the way messages are conveyed widely distributed and acclaimed in many but easy to handle, the embarrassment of and received. Learning how to say ‘No’ for “hot flushes”, and the sudden feeling of “I good reason, being assertive without being developing countries. can’t carry on”. When one is young, one aggressive and appearing co-operative help never imagines that declining levels of oestr- establish rapport and are conducive to better l An electronic version of “Update” including ogen can lead to so much emotional trauma. collaboration with colleagues and students. back issues is now available – you can read Having to work with a variety of When in a position of responsibility, it on your computer screen (using suitable people: surgeons, nurses, technical staff and back your staff and colleagues. Do not jump free software), and download and/or print other anaesthetists can be pleasant and to conclusions. Do not magnify mistakes or all or part of it for reference. fulfiling. However, there is also the potential minimise successes. Never let your staff in our close working environment for down: their trust and faith in you is l If you have an Internet connection you can difficult interpersonal relationships. This is invaluable. It is important that all members more stressful if one has reached a position of a department support each other as access “Update” at of responsibility. You are responsible for the factions within departments are extremely http://www.nda.ox.ac.uk/wfsa It can be smooth running of the operating rooms, for destructive. viewed with either a graphical browser being diplomatic when there is a confront- Time management is also important (looks prettier) such as Netscape or a text- ation between a surgeon/nurse and a fellow and it should be understood that time only browser such as Lynx. anaesthetist, for providing a shoulder for a cannot be expanded infinitely to meet junior consultant to cry on, for knowing all demands. Preserve personal time, pursue l If you don’t have Internet access but do the answers to a postgraduate’s questions hobbies, indulge in regular physical exercise and, of course, for finding time to deal with and remember to relax. Let these time-outs have a computer, we can post you the same all the administrative load that finds its way help put the stresses of life in their proper material on floppy disk with instructions on to your desk. prospective. use. (N.B. This only applies to developing In addition, when women are It is important to recognise the things countries.) successful in their careers, they can that can be changed and have the courage to unwittingly arouse feelings of jealousy, anger change them, to accept those you cannot l You do not need the latest and most and a sense of unfairness in their male change and to have the wisdom to know the colleagues. It is a tremendous advantage to difference. Knowledge, experience, pre- expensive computer to make use of have a partner who is self assured and planning and an understanding of one’s Electronic Update: a 286-PC should be confident in his own right rather than one limitations are signs of a mature anaesthetist. adequate. If you need technical advice, who feels inadequate and is unsure of As time goes on, we see our influence on the please write to Dr Mike Dobson, Nuffield himself. A husband who feels threatened by work we do, on our colleagues, students and Department of Anaesthetics, John Radcliffe his wife’s success can prove to be very friends. We also see their influence on our Hospital, Oxford, OX3 9DU, UK., or send an difficult to live with. lives and on our outlook on life. Fear of the future is very real. Some The prayer of the mature anaesthetist Email request to: may be blasé with a feeling of ‘I will be able could be: [email protected] to ride this out’ but more often than not, “Lord give me love and common sense one feels the inadequacies of old age And standards that are high, l An electronic version of “World Anaesthesia advancing and can’t help wondering whether Give me calm and confidence Newsletter” (incorporating “Anaesthesia one’s deteriorating skills will adversely affect And please, lord, a twinkle in my eye.” Worldwide”) including back issues in similar one’s patients. Loss of a beloved partner at format is also now available at the same this stage is also very traumatic. Financial This essay is based on a talk given at the World security and independence are as vital to a Congress of Anaesthesiology, Montreal, 2000 Internet site. 5 A Message from Albania Dr Aposotol Vaso practice and used what were Anaesthesiology Department then the most modern Trauma Centre general and regional Central Military Hospital anaesthetic techniques. In the Tirana mid-1960’s he was joined by Albania Dr Besim Elezi who was the Email: [email protected] first Albanian to be trained in anaesthesia in Western Albania is an often forgotten Europe, in Denmark. He country of 28,00 sq. km (a little subsequently left anaesthesia bigger than Israel) on the west to become the spiritual and coast of the Balkan peninsula, north of scientific leader of surgery in Greece and separated from Italy by the Albania. Adriatic Sea. The population is 3.3 million The 1970’s saw a generation of We have a limited range of drugs and the official language is Albanian, an doctors trained in Eastern Europe and the available: thiopentone, suxamethonium, Indo-European language that has little in Peoples Republic of China. Among them pancuronium, fentanyl and morphine. We common with other European languages. was another surgeon, Dr Maksut Drrasa, also have nitrous oxide and halothane. Historically, Albania was part of the who was the first to introduce epidural Medical textbooks are also in short supply Roman and then the Byzantine Empire. For anaesthesia into routine practice. In the and only a very limited range of books over five hundred years until independence late 1970’s and early 1980’s, a cohort of and journals can be found in the in 1912, it was part of the Turkish Ottoman anaesthesiologist trained at the University university library. There are no anaesthetic Empire. From the end of the World War II of Tirana started to enter practice and only textbooks or journal written in Albanian. until 1990, it was one of the most extreme then was it possible to introduce a Through the initiative of Dr Mihal and isolated communist states in the world. comprehensive anaesthetic service for the Kerci, a conference on Anaesthesia and Today, it is a parliamentary democracy with whole country. Intensive Care will be held in the Albanian Tirana, a city of approximately 500,000, as A Department of Anaesthesia was Trauma Centre in Tirana in September the capital. established at Tirana University headed by 2000. The Tirana Trauma Centre has a 14- In the last ten years, since the fall of Dr Tritan Shehu who, ten years later, bedded ITU, 10 operating theatres, 13 communism, our country has undergone became the first Professor of Anaesthesia anaesthesiologists and about 60 general, massive social and economic changes that in Albania. He also established the orthopaedic, neuro- and vascular surgeons. have been made more difficult by the Albanian Association of Anaesthesiology Cardiac, paediatric, plastic and other turmoil in our large neighbour, the former in 1993 but, because of adverse surgical specialties are practised at the other Republic of Yugoslavia. The health care circumstances, it is yet to organise a affiliated university hospitals in Tirana. system has not been immune to these conference or publish a journal. Despite the difficulties outlined changes and, although still under state The training of anaesthetists is above, Albanian anaesthesiologists control, now has an insurance-based and a organised by the Ministry of Health in co- provide anaesthesia for a wide range of private sector. operation with the University of Tirana. surgical procedures and have a heavy Although Albania’s only Medical Training lasts four years and encompasses workload. They try to keep up to date School was founded in 1952, the practice theoretical and practical aspects of anaesthesia with progress in the specialty and apply of anaesthesia dates back to the 1920’s and is undertaken in the central hospitals of modern methods and techniques when Austrian and Italian surgeons used Tirana. Unfortunately, the trainees have only whenever they can. ether and regional anaesthesia in the Civil old, and by western standards, very out-dated I wish to express my thanks to Dr Hospital in Tirana. Dr Shiroka, the equipment at their disposal. Most intensive Turchetta from Italy who has helped us pioneer of modern surgery in Albania used care units lack basic equipment such as ECG make contact with the WFSA and these methods, as did other Albanian monitors, oximeters and capnographs and we supplied us with “Update” and to my surgeons who trained in Austria and Italy. can only monitor the pulse and blood colleagues Drs Mihallaq Prifiti, Maksut Endotracheal anaesthesia was introduced pressure manually. Our trainees, therefore, Drrasa and Mihal Kerci helped me prepare in the 1950’s, again by surgeons. have little opportunity to put their theoretical this article on anaesthesia in our country. I In 1961, the first specialist Albanian knowledge into practice and it is impractical would be more than happy to answer any anaesthetist, Dr Mihallaq Prifti, who had for them to attempt to undertake scientific questions or correspond with anyone who trained in St Petersburg in Russia, entered research. contacts me at the above address. 6 A History of Anaesthesia Services in Eritrea hospitals in Asmara moving from one to another. As Ethiopia increased its control over Eritrea, Italian health personnel were systematically marginalised and finally worked only in hospitals caring for the Italian community. They were replaced by doctors who came from the socialist block of Eastern Europe, from the Philip- pines, Israel, Egypt, Sudan and also some from Ethiopia itself and the Italian At the same time, the demand for nuns were mostly replaced by Eritrean nurses. anaesthetists was increasing and three years In 1963, Dr. Gose started a nine – month later in 1969, the Ministry of Health of Ethiopia course in anaesthesia at the then Princess decided to gather all those who were working Tsehai Haileselasse Hospital in Addis Ababa as anaesthesia assistants through out the Kessete Teweldebrhan and two nurses from Eritrea; namely Mengistu country and gave them a six month intensive Health Science Institution Iasu and Bekit Hagheray completed the course training course to try and increase the number PO Box 4947 and returned to work in Asmara. They would and quality of practising anaesthetists. Three Asmara also take it in turn to work in the hospital in of the participants were from Eritrea and Eritrea Massawa for a week or a month at a time. returned there at the end of their course. In The history of anaesthesia in the emerging Later, a Bulgarian anaesthesiologist was addition, the government of Ethiopia decided to state of Eritrea is inextricably linked with employed and in 1969, she was asked (by the open its own school of anaesthesia for nurses the history of its colonial occupation. Italy Eritrean Health Authorities) to train her own in the capital. I was selected by the Minister of occupied Eritrea for 50 years up and until 1942 anaesthesia assistants. Three nurses, namely, Health to establish the school of anaesthesia and the Italians, doctors, nurses and catholic Yosief Michael, Araya G/Tensae and Asmelash and became its first director in September nuns, together with their indigenous assistants G/Mariam were on the initial course. A short 1982. In the 10 years that followed, 8 nurses ran all health services. time after they completed of the course, from Eritrea trained in anaesthesia. . Two of During the British occupation which Asmelash was taken to Addis Ababa and a them subsequently died and one went abroad followed (1942 – 1952), health services were little later, Araya joined the Eritrean Liberation but the remainder are currently working in run by the British Colonial Administration but Struggle to fight for Eritrean independence. Eritrea. incorporated existing services run by Italians Anaesthetists continued to be in very After Eritrea gained its independence who stayed behind in Eritrea (after the defeat short supply in both Eritrea and Ethiopia so in from Ethiopia in 1993, those who had received at of Italy). The latter provided most health 1974, the Ministry of Health of Ethiopia and anaesthesia training in the field during the care for the civilian population through catholic the World Health Organisation (WHO) jointly Liberation Struggle were given up-grading mission clinics and hospitals. opened a School of Anaesthesia at the Duke of courses and were licensed as nurse When the British left in 1952, Eritrea Harar Hospital (now Tikur Anbessa Hospital) in anaesthetists. A further group of 16 nurses became a Trust Federation with its own Addis Ababa under the directorship of Dr. was given a one-year course in anaesthesia in government administering internal affairs Hermann Waldvogel from Switzerland. 1996 run jointly by Simon Haile and within a Federation with Ethiopia. Health Eighteen nurses were enrolled in the initial Ghebrebrhan Haile in 1996. Following this, a service remained based on the Italian colonial course including the author. However, at the national survey on the quality and range legacy although additional doctors were end of the course in 1976, I was not allowed to anaesthesia services in Eritrea was undertaken employed from Germany and the European return to Eritrea but was assigned to work in in late 1998. Based on the results of this socialist block. The most significant thing that Nekemt (Western Ethiopia). Simon Haile and survey, a workshop was organised in took place during this period was the opening Habte Hailemelekot (two of my fellow Eritrean December 1998 by the Department of Human of the Itegue Menen School of Nursing, now nurse anaesthetists) soon left their Resources Development of the Ministry of the Asmara School of Nursing which was assignments in northern Ethiopia and joined Health of Eritrea. At this workshop, it was opened in collaboration with the American the Eritrean Liberation Struggle and started to decided that Ghebrebrhan Haile and myself “Point – 4” Aid programme in 1955. train others in the liberation army in prepare a curriculum for a two-year course in In 1962, Ethiopia annexed Eritrea and the anaesthesia. The WHO-sponsored school of anaesthesia for nurses. This was done and the Ethiopian Ministry of Health ran the Eritrean anaesthesia in Addis Ababa closed soon after new nurse anaesthetist training programme Health Service. At this time, the only qualified because of the Marxist revolution that was officially opened with the enrolment of anaesthetist in Eritrea was Dr. Leonardo Silla overthrew the Ethiopian emperor and the the first batch of 15 students in September who was trained in Italy. He worked in three descent of the country into civil war. 1998. 7 At present Eritrea still has a major Association of Nurse Anaesthetists in 1984. A letter from shortage of nurse anaesthetists and there are The association was originally founded by Dr. no medically qualified anaesthetists in the Herman Waldvogel in 1976 but was dissolved country. Consequently there is a mismatch by the Marxist Regime in 1978. I was Ethiopia between the increasing demands of an privileged to serve as president of the society expanding health service and the anaesthesia for four terms. work force. However, there is a strong In 1989, I was sent to the U.S.A. for determination to solve this problem although further training and after getting my degree in Testahun Fetene Desta we still lack basic teaching aids, books and 1991, I returned to the school of Anaesthesia East Gojjam journals and need more teaching staff. with an American professional license and an Region 3 However, I am sure that we will achieve much expectation that I could continue to be an Debremarcos Hospital in the near future. agent for change by continuing to educate PO Box 37 Some of you who know me from the first nurse anaesthetists and by so doing, be able to Ethiopia WFSA Refresher Course in Nairobi, Kenya or decrease the mortality and morbidity of the the first Symposium for Nurse Anaesthetists surgical population in general and of women Iam a nurse anaesthetist and work at a which was held in Lucerne, Switzerland or who and children in particular. district hospital in the Bahir Dar region have read what I have previously written about After my colleagues and I had trained of Ethiopia, north of Addis Ababa, the my long-term plans for anaesthesia in Ethiopia over 180 nurse anaesthetists, in June 1998, I capital. It is a fertile low-lying area where may ask what am I doing in Eritrea and why I was suddenly ordered to take leave and on tea, coffee, sugar cane, maize and a range of have abandoned my plans for anaesthesia in August 21 1998, my passport and other fruits are grown. The population of the reg- Ethiopia. A little biographical detail may be of documents were confiscated and I was ional is over 200,000 and the administrative value. deported from Ethiopia with two of my language of the region is Amharic. Malaria, I was born to a small farming family in children. I was forced to leave my wife and upper respiratory tract infections, TB, intes- Eritrea in 1946 and was brought up there. I another child of 3 years behind. The main tinal parasites and tropical skin infections graduated from the School of Nursing in reason for this was the border conflict are the most common health problems. Asmara, the capital of Eritrea, as a Nurse and between Ethiopia and Eritrea and I am of The district hospital was built 26 years Nurse Midwife in 1967. At this time Eritrea Eritrean ethnic origin. My wife and youngest ago but for the last 24 years the operating had been annexed by Ethiopia and the then son were finally deported four months later. theatre has not been used. With the help of Imperial Government of Ethiopia decided to Despite what has happened to me, I colleagues, the theatre was cleaned and we assign all graduating male nurses to other have no resentment towards Ethiopia as I have started to discuss with the hospital Medical provinces of Ethiopia. I was assigned to the worked in the Ethiopian Health Services for Director and through him with the Nekonen Haileselassie Hospital in Harar, more than 30 years. I have a vision that Ministry of Health in our region what could (Eastern Ethiopia). Other then the matron, I transcends ethnic origins and political be done about the absence of anaesthetic was the first nurse and nurse midwife to be boundaries and believe that we in the health drugs, equipment and medical gases. It was assigned to the biggest hospital in the professions should remember that bacteria, resolved to try and obtain the necessary province. I worked day and night as the nurse protozoa and viruses recognise no such drugs and equipment although this was in charge of the surgical and maternity wards, boundaries. likely to take many months. as an operating room assistant to the surgeons My ultimate wish is to see peace and As I was determined to make the and obstetricians as well as attending difficult harmony return to the Horn of Africa, so that theatre operational as soon as possible, I deliveries, collecting blood for transfusion we anaesthetists can organise ourselves at a decided to make the long journey to Addis whenever it was necessary and undertaking regional level, host Regional Scientific Ababa, some 400km, to try and obtain administrative duties. Mothers in obstructed Symposia and work towards the WFSA goals what we needed. I would like to thank those labour and those with foetal distress were of “safe anaesthesia for all” by conscientiously hospitals in Addis that understood my diffi- frequently referred to our hospital from places discharging our professional responsibilities culties and helped by donating drugs, airways which were 70 – 12O km. away because there like our colleagues in other regions of Africa and endotracheal tubes. On my return, we was no one with anaesthetic skills in the and beyond. were able to start surgery and now perform referring hospitals. Many of the mothers died 15-20 emergency operations each month. due to ruptured uterus or sustained permanent Editorial Note: Most of these are on pregnant women or for injuries such as vesico-vaginal fistulae. I Eritrea regained its independence from bowel obstruction or appendicitis. therefore decided to study anaesthesia and be Ethiopia in 1993. It has an area of 121,300 Our staff consists of one surgeon, part of the solution. sq km (approximately half the size of the UK) provided by MSF for one year, one trained In 1974, I joined the WHO-sponsored and a population of 3.9 million. It is one of nurse, two health assistants and me, a nurse School of Anaesthesia in Addis Ababa and six the poorest countries in the world with a per anaesthetist. When we operate the nurse years later in September 1982, I was able to capita GDP of $660. Life expectancy is scrubs, one health assistant acts as a surgical found and become the director of the Ethiopian approximately 55 years and infant mortality is assistant and the other as a runner. All are School of Anaesthesia for Nurses, a position I 76/1,000. A cease-fire and truce was finally trained to apply cricoid pressure and can held for almost 17 years. I was also agreed in the border war between Ethiopia assist me when necessary. We are all on duty instrumental in resurrecting the Ethiopian and Eritrea in June 2000. 24 hours/day. 8
Description: