Table Of ContentForm Approved
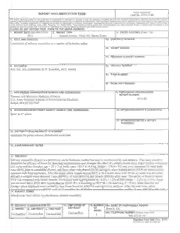
REPORT DOCUMENTATION PAGE
OMB No. 0704-0188
The public reporting burden for this collection or information is estimated to average 1 hour per response, including the time for reviewing instructions, searching existing data sources.
gathering and maintaining the data needed, and completing and reviewing the collection of information. Send comments regarding this burden estimate or any other aspect of thrs collection of
information. including suggestrons for reducing the burden. to Department of Defense, Washington Headquarters Services. Directorate for Information Operations and Reports (0704·0188).
1215 Jefferson Davis Highway, Suite 1204. Arlington, VA 22202-4302. Respondents should be aware that notwithstanding any other provision of law, no person shall be subject to any
penalty for failing to comply with a collection of information if it does not display a currently valid OMS control number.
PLEASE DO NOT RETURN YOUR FORM TO THE ABOVE ADDRESS.
1. REPORT DATE (00-MM-YYYY) REPORT TYPE 3. DATES COVERED (From- To)
,2.
2011 Journal Article -Med. Sci. Sports Exerc.
4. TITLE AND SUBTITLE 5a. CONTRACT NUMBER
Limitations of salivary osmolality as a marker of hydration status
5b. GRANT NUMBER
5c. PROGRAM ELEMENT NUMBER
6. AUTHOR($) 5d. PROJECT NUMBER
B.R. Ely, S.N. Cheuvront, R.W. Kenefick, M.N. Sawka
5e. TASK NUMBER
5f. WORK UNIT NUMBER
7. PERFORMING ORGANIZATION NAME(S) AND ADDRESS(ES) 8. PERFORMING ORGANIZATION
REPORT NUMBER
Thern1al and Mountain Medicine Division
M10-44
U.S. Army Research Institute of Environmental Medicine
Natick, MA 01760-5007
9. SPONSORING/MONITORING AGENCY NAME(S) AND ADDRESS(ES) 10. SPONSOR/MONITOR'S ACRONYM(S)
Same as #7 above.
11. SPONSOR/MONITOR'S REPORT
NUMBER(S)
12. DISTRIBUTION/AVAILABILITY STATEMENT
Approved for public release; distribution unlimited
13. SUPPLEMENTARY NOTES
14.ABSTRACT
Salivary osmolality (Sosm) is a potentially useful hydration marker but may be confounded by oral artifacts. This study aimed to
determine the efficacy of Sosm for detecting hypohydration and evaluate the effect of a simple mouth rinse. Eight healthy volunteers
(six males and two females; age= 22 ± 7 yr, body mass= 83.7-± 14.9 kg, height= 176.9 ± 9.2 em) were measured for nude body
mass (BM), plasma osmolality (Posm), and Sosm when euhydJ·ated (EUH) and again when hypohydrated (HYP) by exercise-heat
exposure with fluid restriction. After the initial saliva sample during HYP, a I 0-s mouth rinse with 50 mL of water was provided,
and saliva samples were obtained I min (RINO 1) , 15 min (RJN 15), and 30 min (RIN30) after rinse. The ability of Sosm to detect
HYP was compared with Posm. Results: Volunteers were hypohydrated by -4.0% ± 1.2% ofBM (range= -2.2% to -5.3%). Sosm
was elevated above EUH after hypohydration (EUH 58± 8 mmol•kg vs HYP 96 ± 28 mmol-kg, P < 0.05). Sosm baseline and
change values displayed more variability than Posm based on ANOVA and regression analyses. After the oral rinse, saliva
.J. • · .· rn n. rfl t c ..., n t1 r.c· . .. .. .·. . .. • .. · • · 1 c , · Inn. < 1 f\ ")<;
15. SUBJECT TERMS
dehydration; fluid intake; hypohydration; plasma osmolality
16. SECURITY CLASSIFICATION OF: 17. LIMITATION Oi= 18. NUMBER 19a. NAME OF RESPONSIBLE PERSON
a. REPORT b. ABSTRACT c. THIS PAGE ABSTRACT OF Brett R. Ely
PAGES
Unclassified 19b. TELEPHONE NUMBER (Include area code)
Unclassified Unclassified Unclassified 5
508-233-4 I 34
Standard Form 298 (Rev. 8/98)
Prescribed by ANSI Std. Z39. 18
Limitations of Salivary Osmolality as a Marker
of Hydration Status
BRETT R. ELY, SAMUEL N. CHEUVRONT, ROBERTW. KENEFICK, and MICHAEL N.SAWKA
U.S. Army Research Instituteof Environmental Medicine, Natick, MA
ABSTRACT
ELY,B.R.,S.N.CHEUVRONT,R.W.KENEFICK,andM.N.SAWKA.LimitationsofSalivaryOsmolalityasaMarkerofHydration
Status.Med.Sci.SportsExerc.,Vol.43,No.6,pp.1080–1084,2011.Salivaryosmolality(S )isapotentiallyusefulhydrationmarker
osm
butmaybeconfoundedbyoralartifacts.Purpose:ThisstudyaimedtodeterminetheefficacyofS fordetectinghypohydrationand
osm
evaluatetheeffectofasimplemouthrinse.Methods:Eighthealthyvolunteers(sixmalesandtwofemales;age=22T7yr,bodymass=
83.7T14.9kg,height=176.9T9.2cm)weremeasuredfornudebodymass(BM),plasmaosmolality(Posm),andSosmwheneuhydrated
(EUH)andagainwhenhypohydrated(HYP)byexercise–heatexposurewithfluidrestriction.AftertheinitialsalivasampleduringHYP,
a10-smouthrinsewith50mLofwaterwasprovided,andsalivasampleswereobtained1min(RIN01),15min(RIN15),and30min
(RIN30)afterrinse.TheabilityofSosmtodetectHYPwascomparedwithPosm.Results:Volunteerswerehypohydratedbyj4.0%T
1.2%ofBM(range=j2.2%toj5.3%).SosmwaselevatedaboveEUHafterhypohydration(EUH58T8mmolIkgj1vsHYP96T
28 mmolIkgj1, P G 0.05).Sosm baseline and changevalues displayedmore variability than Posm based on ANOVA and regression
analyses.Aftertheoralrinse,salivadecreasedinconcentration(RIN01=61T17mmolIkgj1,PG0.05)butreturnedtoprerinsevalues
within15min(RIN15=101T25mmolIkgj1)andremainedsimilar30minafter(RIN30=103T33mmolIkgj1).Conclusions:Sosmwas
remarkablyaltered1minafterabriefwatermouthrinse.Fifteenminutesprovedanadequaterecoverytime,indicatingthatthetiming
oforalartifactsandsalivasamplecollectioniscriticalwhenconsideringS forhydrationassessment.Giventheinherentvariability
osm
and profoundeffect of oral intake, use of S as a markerof hydrationstatus isdubious.Key Words:DEHYDRATION, FLUID
osm
INTAKE,HYPOHYDRATION,PLASMAOSMOLALITY
T
S he noninvasive ease with which saliva samples can to optimize performance in warm–hot conditions (14), Sosm
E be obtained makes their use ideal to study physio- mayprovideausefulmeasureforscreeninghydrationstatus.
C
N logical functions during occupational, athletic, or During athletic competitions and occupational and mili-
E militarytasks.Salivaryosmolality(S )hasbeenproposed tary activities, progressive body water deficits may occur
I osm
C
as a useful marker of hydration status because values in- over time while small amounts of fluid are consumed (e.g.,
S
D crease when dehydration is mediated by sweat loss in con- rest breaks or water stops during a road race). Besides con-
E trolledlaboratorystudies(13,20,21).Althoughnotaswidely suming water, other fluid and food consumption is com-
I
L studiedasotherhydrationassessmentmarkerssuchasblood mon during athletic, occupational, and military tasks. It is
P
P and urine, recent research has shown that S has marked unknown what effect recent fluid and food consumption
osm
A
heterogeneity (4,17) and is a poor diagnostic marker of might have on S . One study presenting limited data
osm
hydration status for high-risk populations such as hospital (n = 4) argued that a simple water mouth rinse (insufficient
patients with fluid–electrolyte imbalances (4). However, in to alter hydration status) seems to dilute saliva and degrade
lower-risk situations (e.g., occupational, sports, and mili- the diagnostic validity of the measures in dehydrated vol-
tary) where concern is focused on maintaining euhydration unteers (4). Those findings raise questions regarding the
effect of consumed beverages (water) on the magnitude,
consistency,anddurationofanyconfoundingeffect.Knowl-
edge of how long S dilution effects persist when a small
osm
amount of fluid is introduced to the oral cavity is a key to
Address for correspondence: Brett R. Ely, M.S., USARIEM, Thermal &
understanding the potential real-world usefulness of S as
MountainMedicineDivision,KansasSt.,Bldg.42,Natick,MA01760-5007; osm
ahydrationmarkerinlower-riskpopulations.
E-mail:[email protected].
SubmittedforpublicationAugust2010. The purposes of this study were to measure Sosm during
AcceptedforpublicationNovember2010. euhydration (EUH) and hypohydration (HYP) and to ex-
amine the effect (magnitude and duration) of a brief mouth
0195-9131/11/4306-1080/0
MEDICINE&SCIENCEINSPORTS&EXERCISE(cid:1) rinseontherecoverykineticsofSosmduringhypohydration.
Copyright(cid:2)2011bytheAmericanCollegeofSportsMedicine It was hypothesized on the basis of laboratory observa-
DOI:10.1249/MSS.0b013e3182058643 tions that Sosm would decline after an oral rinse with water
1080
Copyright © 2011 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.
but recover within 15–30 min. A rapid recovery of S by subtracting day 1 values from day 2 values to determine
osm
would improve its usefulness as a hydration marker for absolutechanges.
lower-risk situations. A water rinse was selected because On the first day of experimental testing (day 3; EUH),
this should have the smallest potential effect on S com- volunteersreportedtothelaboratoryat0630hformeasures
osm
pared with consumption of commercial beverages or food ofnudeBM,P ,U ,andS .Volunteerswerethenfree
osm sg osm
often taken duringphysical activity inwarm–hot weather. to eat and drink ad libitum for the remainder of the morn-
ing. On the afternoon of day 3, volunteers returned to the
laboratory to perform 3–5 h of work/rest cycles (50 min
of work, 10 min of rest) of treadmill (1.56 mIsj1, 4%–7%
METHODS
grade)and/orcycleergometerexercise(100–120W)insidean
Subjects. Eight healthy, active soldier volunteers took environmental chamber set to 40-C, 20% relative humidity
part in this study (six males and two females; (mean T with1mIsj1laminarwindflow.Thepurposeoftheexercise–
SD) age = 22 T 7 yr, body mass = 83.7 T 14.9 kg, height = heat exposure was to increase body heat storage and induce
176.9T9.2cm,bodyfat=23.8%T6.5%).Thesearedifferent sweatingtoproducehypohydration(hypertonic–hypovolemia).
subjects from those in a previous study from our laboratory The range of exposure times, body sizes, and sweating rates
examining P (4). All volunteers passed their most recent allowed for S responses to be examined over a range of
osm osm
Army Physical Fitness Test and received a general medi- hypohydration beyond the threshold of 2% BM loss, where-
cal clearance before participation; thus, all were considered as overnight recovery after these procedures eliminated con-
healthy and physically fit. Use of alcohol, dietary supple- founding factors of varying exercise modality or exposure
ments, and any medication other than an oral contraceptive duration. The magnitude of hypohydration (HYP) selected
wasprohibited.Femalevolunteerswerenotpregnantnordid spanned a functionally important range of 2%–6% of BM
anybecomepregnantduringthestudy.Menstrualcyclephase (7,9,14). In response to exercise–heat exposure, water (sweat,
and oral contraceptive use were not standardized but were urine) volume and BM losses were considered equivalent
considered small sources of added within-subjects biologi- (1 mL = 1 g). The level of body water deficit was calculated
cal variability (4,5,15,19) onthe basis of the study question, fromthecorrected(12)changeinnudeBMduring24h(from
design, and duration. For example, female sex hormones al- 0630 h on day 3 to 0630 h on day 4) and expressed as a
terbaselineP toasimilardegreeasday-to-dayvariability percentage of day 3 EUH BM. The starting 0630 h nude
osm
(È4 mmolIkgj1) (16,19), whereas the P response to de- BM used in the denominator of the calculation was consid-
osm
hydration and rehydration remains the same between men- ered EUH for an individual if it was within T1% BM of his/
strual cycle phases (15,19) and between the sexes (16). her initial 3-d mean and confirmed EUH by measurement of
Volunteers were provided informational briefings and gave Posm and Usg (14). Total body water (TBW) was calculated A
voluntary, informed written consent to participate. Investi- as 0.73 (cid:1) lean body mass + 0.1 (cid:1) fat mass because these P
P
gators adhered to AR 70-25 and U.S. Army Medical Re- relationships are constant throughout adult life (9). Change L
I
search and Materiel Command Regulation 70-25 on the use in TBW was calculated by dividing TBW by BM loss, with E
D
of volunteers in research. The U.S. Army Research Institute the assumption that corrected BM lost through sweating was
S
of Environmental Medicine Human Use Review Committee entirely water. Body composition was assessed using sex- C
approvedthisstudy. specific three-site skinfold measurements and estimated using IE
Experimental design. Each volunteer participated in appropriateformulas(10). N
C
all 4 d of the study protocol. During the initial 3 d, fluid Afterexitingtheenvironmentalchamber,volunteerswere E
intake was prescribed (3 LIdj1), and first morning nude provided with a small, standardized meal (450 kcal; 57% S
body mass (BM) was measured to establish baseline body CHO, 30% fat, 13% protein, 450 mg of Na+) and 200 mL
mass(BM)variability(3,4)whenconsumingadequatefluids of water or apple juice. No additional food or water was
(9). P , S , U , and BM were measured each morn- permitted, and volunteers were kept in supervised housing
osm osm sg
ing on three consecutive days, so that data on biological until morning. On the morning of day 4, nude BM, P ,
osm
variation could be generated using widely applied methods U , and S measures were made once again for
sg osm
(6).Thethirddayofbaselinemeasurements(day3)doubled comparison with day 3 (EUH). The sequence of events for
as the first day of experimental testing (EUH). Volunteers all measurements on days 3 (EUH) and 4 (HYP) remained
were instructed to consume 1 L of premeasured water be- consistent throughout the study. Volunteers reported each
tween waking and 1800 h and another 2 L of prepackaged morningat0630h,wereweighednudeaftervoidingaurine
sportsdrinkforconsumptionbetween1800and2200heach sample for U analysis, and then sat quietly for 30 min
sg
day. Physical activity was restricted to avoid excess body before having their blood drawn and providing a saliva
waterlossesfromsweating.Days1and2werecomparedto sample. Volunteers remained seated through blood and sa-
determine EUH standards for percent change in BM versus liva collection to avoid potentially inducing any postural
change in P and S . Percent change in BM was calcu- fluidshifts(8).
osm osm
lated by the following formula: [(day 2 BM j day 1 BM) / Analyticalmeasures. A3-mLsampleofvenousblood
day1BM(cid:1)100%].P andS weresimilarlycompared was collected without stasis in lithium–heparin tubes
osm osm
LIMITATIONSOFSALIVARYOSMOLALITY Medicine&ScienceinSports&Exercised 1081
Copyright © 2011 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.
(Sarstedt, Inc., Newton, NC) and then centrifuged at 3500g abilitylevel.Goodness-of-fitstatisticswereperformedusing
at 4-C for 10 min, and plasma was immediately separated linear regression analysis to obtain shared variance (r2) and
for analysis. P was measured in triplicate by freezing uncertainty(SEE)inP andS (y)whenassociatedwith
osm osm osm
point depression on a dedicated osmometer (Fiske Micro- acute measures of change (BM) in hydration state (x).
osmometer, Model 210, Norwood, MA) by the same tech- Analyses were computed using GraphPad Prism 5.02 soft-
nician throughout the study. First-void morning urine was ware (GraphPad Software, Inc., San Diego, CA). All data
provided in a sterile, inert polypropylene cup (Tyco Health- are presentedas mean T SD.
care Group, Mansfield, MA), and a small volume was
measured for specific gravity (U ) in duplicate using a re-
sg
fractometer (1110400A TS Meter; AO Reichert Scientific RESULTS
Instruments, Keene, NH). U was selected because it is a
sg Baseline variation in hydration assessment mar-
standard euhydration assessment measure (14) and also be-
kers. The within-subjects CV was G1% for P (0.3%),
i osm
cause it is the least variable of common urine concentration
BM (0.6%), and U (0.5%). The CV for S was almost
sg i osm
measureswhentryingtodetectchange(4).Nudebodymass
seventimeslarger(6.6%).Inallcases,thebetween-subjects
(BM) was measured each morning on a precision platform
CV was larger than the CV, as previously reported for
i
scale (T50 g; Model WSI-600; Mettler Toledo, Toledo, OH), many biological measures (6). All values were very similar
whichwascheckeddailyat25,70,and95kg.
to those recently reported for hydration assessment mark-
Salivasamples. A2-mLsampleofunstimulatedwhole
ers using similarmethodsin a larger study population (4).
saliva was collected for each volunteer on every baseline
Hydration. Allvolunteersbeganexperimentaltestingin
and experimental day. Volunteers produced samples during
a euhydrated state on the basis of meeting two or more hy-
EUH and HYP by allowing saliva to collect in their mouth
drationassessmentcriteria(14)(Table1).Allvolunteershad
overtimeandexpellingitintoasmalltube.Aftercollection
a first-morning nude BM within 1% of their 3-d EUH av-
of the initial 2-mL saliva sample in HYP only, volunteers
erage. Of eight volunteers, five had U G1.020 and two
sg
were given 50 mL of water and instructed to rinse their beganwithP G290mmolIkgj1(14).Ofeightindividuals,
osm
mouth for 10 s without swallowing and then spit the water
six had starting (EUH) S below the suggested dehydra-
osm
back into the cup. One minute later, a second 2-mL saliva tion threshold of 83 mmolIkgj1 (4). No volunteer was con-
samplewascollected(RIN01).Twoadditionalsampleswere
sidered overtly hypohydrated before testing on the basis of
collected at 15 min (RIN15) and 30 min (RIN30) after the
P G297 and U G1.025 (4).
osm sg
oral rinse to track S recovery. The purpose of this rinse
osm Afterexercise–heatstressandfluidrestrictionprocedures,
was to introduce a small amount of fluid to the mouth volunteers were hypohydrated by j4.0% T 1.2% of body
S without any effect on hydration status to examine the po- mass (range = j2.2% to j5.3%), which corresponded to
CE tential confounding effect of fluid in the oral cavity in the j6.8% T 2.0% TBW (range = j4.3% to j9.4%). Table 1
N absence ofswallowing (rehydration).
provides body mass, TBW, and hydration marker values
E Saliva samples were collected into single-use polypropyl-
I when euhydrated and hypohydrated. P , U , and S
C osm sg osm
eneFalcontubes(VoigtGlobalDistribution,Inc.,Lawrence,
S all increased in response to fluid losses as expected. Of
D KS)andimmediatelycentrifugedat3500gat4-Cfor10min eight volunteers in HYP, five surpassed the proposed S
osm
IE before analysis. Sosm was measured immediately after cen- diagnostic threshold for hypohydration of 83 mmolIkgj1
L trifugation by freezing point depression by the same tech-
P (4), whereas seven surpassed the proposed threshold for
AP nician on the same osmometer (Fiske Micro-osmometer, Posmhypohydration of 297 mmolIkgj1 (4).
Model210)tominimizevariabilityintechnique.Allsamples
Figure 1 plots the individual percent change in BM and
were run in triplicate, and the median value was taken as
TBW versus P (A) and S (B) during HYP. Shared
osm osm
final. If any of the intrasample triplicate S measures de-
osm variance was approximately 75% for associations between
viatedby93%,twomoresampleswererun,andthemedian change in absolute P and change in BM or TBW (r =
osm
of five values was used. The analytical coefficient of varia- j0.85to0.87),whereassharedvariancewasapproximately
tion(CV)forthetriplicatemedianvalueswas1%. 50% for S (r = j0.71 to 0.73) when associated with
osm
Statistics. S values for EUH, HYP, RIN01, RIN15,
osm change in BM or TBW. Similar trends were seen when
and RIN30 were compared using a one-way repeated-
percent changes in BM and TBW were compared with the
measures ANOVA. Tukey post hoc procedure was used
when a significant F value occurred. Previous work us-
ing the same test method (4) showed an approximate 10% TABLE1.BM,TBW,P ,U ,andS duringEUHandHYP.
osm sg osm
within-subjects CV for Sosm (È7 mmolIkgj1) and 950% EUH HYP
(935 mmolIkgj1) rise in Sosm between EUH and HYP. BM(kg) 83.8T14.8(69.5–109.8) 80.4T13.7(67.2–104.5)
Asamplesizeofeightvolunteerswasdeterminedsufficient TBW(kg) 48.8T10.0(36.2–63.7) 45.3T8.9(34.7–58.4)
(18) to detect large (935 mmolIkgj1) changes in S . Posm(mmolIkgj1) 291T3(285–293) 303T7(294–315)
Differences in Sosm G10 mmolIkgj1 were considered mosamr- USossgm(mmolIkgj1) 1.05188TT80.0(5005–(711.0)10–1.024) 1.09268TT02.800(370(–11.05242)–1.032)
ginal a priori. Significance was accepted at the 95% prob- ValuesdisplayedaremeanTSD(range).
1082 OfficialJournaloftheAmericanCollegeofSportsMedicine http://www.acsm-msse.org
Copyright © 2011 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.
hydration status because of the ease of collection in real-
world scenarios. However, S has only been tested in
osm
controlled laboratory conditions, which are unlikely to
mimic real-life fluid consumption and eating patterns typi-
cally encountered during actual occupational, sports, or
militarymedicineuse.Thepresentstudycarefullymeasured
hydrationstatusandS andexperimentallyexaminedday-
osm
to-day variability and effect of mouth rinse on S . The
osm
collected information is important in determining whether
S might be used as a hydration marker in real-life, low-
osm
risk situations. The primary findings of this investigation
were as follows: 1) S enabled distinction between EUH
osm
and HYP conditions in most well-controlled cases, 2) S
osm
demonstrated considerable variability in day-to-day mea-
surement and in magnitude of response to HYP, 3) S
osm
is easily confounded after a brief oral rinse, but 4) S
osm
values recoveredwithin 15min ofrinsing.
S increased in all eight volunteers in response to fluid
osm
losses of 2.2%–5.3% body mass (4.3%–9.4% body water
loss),which matches previous studies wherehypohydration
in the range of 2%–7% body mass reliably increased S
osm
(4,20,21). However, shared variance was less, and the SEE
was much larger between the level of dehydration and ei-
ther the absolute S (Fig. 1B) or its change compared
osm
with P (Fig. 1A). This is likely explained by large var-
osm
iability in S between subjects (4,17). Thus, S is an
osm osm
imprecise discriminator between levels of hypohydration
FIGURE1—P (A)andS (B)valuesduringEUHandHYPplot- (mild(È2% BM loss) versus moderate tosevere (Q4% BM
osm osm
tedagainstpercentchangeinbodymassandTBW,withbest-fitlinear loss)) when examined in cross section. When serial S
osm
regressionforeach.
samples were taken from individuals undergoing progres-
sive hypohydration during a single test session, a much A
change in P (r = j0.87) and S (r = j0.71) from strongerrelationshiphasbeenreported(e.g., r=0.94)(18). P
EUH to HYoPsm. The SEE for salivoasm(19–20 mmolIkgj1) However,day-to-dayvariabilityinSosmwasnearly10times PL
I
was four to five times larger than that for plasma (4– larger in this and other studies (4) than P , BM, or U . E
4.6 mmolIkgj1) whether comparing absolute or change A recent work (4) also showed that aossmignificant nosng- D
S
values. uniformity of variances within subjects would make daily C
Salivary osmolality recovery dynamics. Figure 2 Sosm change monitoring of questionablediagnosticvalue. IE
presents the influence of a water rinse on S values dur- S was confounded by a brief oral rinse with water N
osm osm C
ing a 30-min period. After the oral rinse, Sosm values de- 1 min after rinse, resulting in values no different from E
creased(PG0.05)toEUHlevels,despitenofluidintakeor S
change in hydration status. Only one S value remained
osm
over the proposed diagnostic threshold for hypohydration
of 83 mmolIkgj1 (4) after the oral rinse (RIN01 = 61 T
17 mmolIkgj1). Fifteen minutes later, S values had
osm
returned to the prerinse HYP values, with six of eight val-
ues surpassing the proposed diagnostic threshold for hy-
pohydration (4). Values were nearly identical at 15 min
(RIN15=101T25mmolIkgj1)and30min(RIN30=103T
33 mmolIkgj1)after rinse.
DISCUSSION
Measuring and maintaining hydration state has impor-
tant implications for health and performance, but a simple, FIGURE 2—Sosm values (mean T SD) during EUH, HYP, 1 min
(RIN01), 15 min (RIN15), and 30 min (RIN30) after oral rinse. Dot-
noninvasive, and accurate measure of hydration status re-
ted line denotes the proposed dehydration diagnostic threshold of 83
mains elusive (1). Sosm has been proposed as a marker of mmolIkgj1(4).*SignificantlydifferentfromEUHandRIN01.
LIMITATIONSOFSALIVARYOSMOLALITY Medicine&ScienceinSports&Exercised 1083
Copyright © 2011 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.
EUH and well below the threshold for HYP (4), despite assessment in real-world scenarios. Future research may
no change in hydration status. However, most values re- examine additional possible confounding scenarios such
covered within 15 min of rinsing (Fig. 2), indicating that as recent exercise, carbohydrate–electrolyte beverage con-
15 min is an adequate time standard for field use between sumption, and even the ability of S to distinguish between
osm
water consumption and saliva sampling. Sports drinks, euhydration and hyperhydration or hyponatremia, a serious
food, or gum may contain numerous factors (carbohydrate, riskinendurancesportingevents.
Na+, K+, etc.) that are likely to additionally confound S In conclusion, a brief oral rinse easily confounds S
osm osm
results. As a result, the practical usefulness of S may be measurement during hypohydration, indicating that S
osm osm
limited in a real-world scenario where athletes or soldiers is of limited use for hydration assessment when fluids are
are consuming fluids, eating, chewing gum or tobacco, and regularly being consumed. Although S values recover
osm
smoking. The effect of other oral intake has not yet been within 15 min of oral intake, timing of fluid intake is para-
examined, although all of these confounders are likely to mount in obtaining a valid measure of hydration status
affect S outcomes. through S . Given the inherent variability and profound
osm osm
Another potential consideration in addition to oral intake effect of oral intake on S , its use as a marker of hydra-
osm
is the effect of aerobic and anaerobic exercises on S . tion statusis dubious.
osm
Salivary Na+, K+, and protein concentrations have all been
found to increase after a bout of exercise (2,11). Changes
in blood flow to the salivary glands and catecholamine- Theopinionsorassertionscontainedhereinaretheprivateviews
oftheauthor(s)andarenottobeconstruedasofficialorasreflecting
induced shifts of water from circulation can also affect
theviewsoftheArmyortheDepartmentofDefense.
Sosm without a meaningful change in hydration status. In Theauthorshavenofundinginformationtodisclose.
athletic events, labor, and military operations, physical ac- The authors thank the volunteers who donated their time and
efforttoparticipateinthisstudy.
tivity may further confound S and must also be consid-
osm Theresultsofthepresentstudydonotconstituteendorsement
ered in examining the applicability of Sosm for hydration bytheAmericanCollegeofSportsMedicine.
REFERENCES
1. ArmstrongLE.Assessinghydrationstatus:theelusivegoldstan- 13. OliverSJ,LaingSJ,WilsonS,BilzonJL,WalshNP.Salivaindices
dard.JAmCollNutr.2007;26:575S–84S. track hypohydration during 48 h of fluid restriction or combined
2. Ben-AryehH,RollN,LahavM,etal.Effectofexerciseonsali- fluidandenergyrestriction.ArchOralBiol.2008;53:975–80.
varycompositionandcortisolinserumandsalivainman.JDent 14. Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ,
Res.1989;68(11):1495–7. Stachenfeld NS. American College of Sports Medicine. Position
S
E 3. CheuvrontSN,CarterRIII,MontainSJ,SawkaMN.Dailybody Stand: exercise and fluid replacement. Med Sci Sports Exerc.
C massvariabilityandstabilityinactivemenundergoingexercise– 2007;39(3):377–90.
N
heatstress.IntJSportsNutrExercMetab.2004;14:532–40. 15. Stachenfeld NS, Silva C, Keefe DL, Kokoszka CA, Nadel ER.
E
I 4. Cheuvront SN, Ely BR, Kenefick RW, Sawka MN. Biological Effects of oral contraceptives on body fluid regulation. J Appl
C
variation and diagnostic accuracy of dehydration assessment Physiol.1999;87(3):1016–25.
S
markers.AmJClinNutr.2010;92:565–73. 16. StachenfeldNS,SplenserAE,CalzoneWL,TaylorMP,KeefeDL.
D
5. Fraser CG. Biological Variation: From Principles to Practice. Sex differences in osmotic regulation of AVP and renal sodium
E
I Washington(DC):AACCPress;2001.p.1–151. handling.JApplPhysiol.2001;91(4):1893–901.
L
P 6. FraserCG,HarrisEK.Generationandapplicationofdataonbio- 17. Taylor NAS, van den Heuvel AMJ, Kerry P, et al. The efficacy
P logical variation in clinical chemistry. Crit Rev Clin Lab Sci. of saliva osmolality as an index of hydration state: is it worth
A
1989;27:409–37. the spit? In: Proceedings of the 13th International Conference
7. GreenleafJE.Problem:thirst,drinkingbehavior,andinvoluntary onEnvironmentalErgonomics;August2–7,2009:Boston(MA).
dehydration.MedSciSportsExerc.1992;24(6):645–56. p.279–82.
8. Hagan RD, Diaz FJ, Horvath SM. Plasma volume changes with 18. Tran ZV. Estimating sample size in repeated measures analysis
movement to supine and standing positions. J Appl Physiol. ofvariance.MeasPhysEducExercSci.1997;1(1):89–102.
1978;45:414–8. 19. Vokes TJ, Weiss NM, Schreiber J, Gaskill MB, Robertson GL.
9. Institute of Medicine. Dietary Reference Intakes for Water, Po- Osmoregulationofthirstandvasopressinduringnormalmenstrual
tassium, Sodium, Chloride, and Sulfate. Washington (DC): Na- cycle.AmJPhysiol.1988;254(23):R641–7.
tionalAcademiesPress;2005.p.73–185. 20. Walsh NP, Montague JC, Callow N, Rowlands AV. Saliva flow
10. JacksonAS,PollockML.Practicalassessmentofbodycomposi- rate,totalproteinconcentrationandosmolalityaspotentialmark-
tion.PhysSportsMed.1985;13:76–90. ersofwholebodyhydrations statusduringprogressive acutede-
11. LjungbergG,EricsonT,EkblomB,BirkheadD.Salivaandmar- hydrationinhumans.ArchOralBiol.2004;49:149–54.
athonrunning.ScandJMedSciSports.1997;7:214–9. 21. WalshNP,LaingSJ,OliverSJ,MontagueJC,WaltersR,Bilzon
12. Mitchell JW, Nadel ER, Stolwijk JAJ. Respiratory weight losses JL.Salivaparametersaspotentialindicesofhydrationstatusdur-
duringexercise.JApplPhysiol.1972;32:474–6. ingacutedehydration.MedSciSportsExerc.2004;36(9):1535–42.
1084 OfficialJournaloftheAmericanCollegeofSportsMedicine http://www.acsm-msse.org
Copyright © 2011 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.